
Health anxiety also called illness anxiety disorder or “health anxiety OCD” by some clinicians, is a persistent fear of having or developing a serious disease even when exams, labs, and imaging are reassuring. People with health anxiety often misread normal and occasional sensations (a fluttering heart, a headache, a tight chest) as signs of worry.
The self-imposed worry can dominate daily life, strain relationships, and send someone into cycles of checking, medical consultations, and the never-ending loop of late-night internet research.
Two patterns commonly appear:
- Care-seeking: frequent appointments, multiple specialists, repeated testing.
- Care-avoidant: avoiding clinics, news, or medical shows for fear of bad news, yet remaining preoccupied with the symptoms and health worries.
It is very important to note that this isn’t “faking” or “attention-seeking.” The fear feels real, and reassurance rarely sticks for long. If this resonates with you or is positive in your loved one, it is time to seek professional care.
How Health Anxiety Looks: Day to Day & Common Symptoms
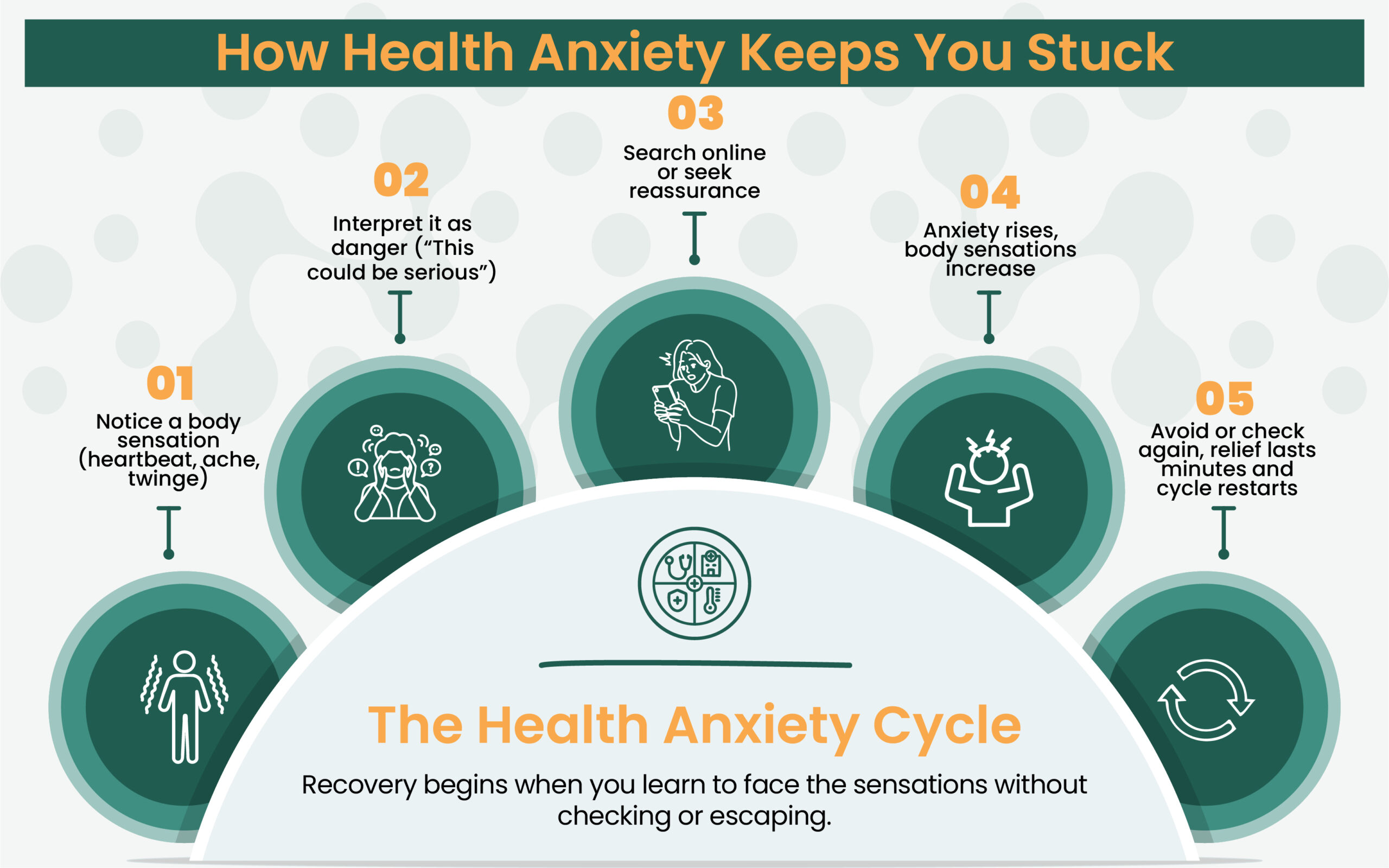
A vivid pattern of the feelings many health anxiety-positive people describe: noticing a twinge, googling rare conditions, feeling surges of panic, and then doubling down on checking and medical research. In short, the more they scan their body, the more sensations they notice, and the scarier it feels.
Typical Symptoms include:
- Constant worry about health; being easily alarmed by benign sensations.
- Repeatedly checking the body (lumps, moles, pulse, temperature) or ruminating about symptoms.
- Searching for symptoms online, hopping between doctors, and having difficulty accepting normal tests.
- Avoiding activities “just in case,” or acting as if ill (skipping exercise, travel, work).
- Seeking reassurance from loved ones over and over, then doubting the answer minutes later.
- Somatic anxiety signs, headache, palpitations, nausea, and tingling further fuel the fear.
With CPG, Reclaim Calm, Not Just Reassurance
Health anxiety doesn’t vanish with one normal test; it fades when you learn how to live with uncertainty confidently. Start therapy that teaches your mind to step out of the “what if” spiral.
Why it Happens (Causes, Risks, and Triggers)
There isn’t a single cause; several factors tend to stack and contribute to health anxiety:
- Beliefs about health and uncertainty. If every unfamiliar sensation is judged “serious until proven otherwise,” worry spikes and sticks.
- Family and learning history. Caregivers who worry constantly about health, or a childhood spent around serious illness, can shape how the brain treats normal sensations.
- Life stressors and losses. Illness in someone close, a difficult diagnosis, scare, parenthood, job strain, or trauma commonly precede the onset.
- Overlap with other conditions. Health anxiety often travels with Generalized Anxiety Disorder, Panic Disorder, Illness Anxiety OCD, or somatic symptom disorder. Panic-prone people, for example, misinterpret surges of arousal as medical danger; health anxiety broadens that fear to many sensations and diseases.
- Work exposure. People immersed in severe illness, ICU staff, and first responders can develop persistent preoccupation and even PTSD. Regular contact with rare tragedies skews risk perception and feeds compulsive checking and internet research.
Expert Insight
- People often describe a personal spiral: discovering a benign lump after a cold, then hours of reading survival statistics, panic at night, then another round of testing, then a new symptom.
- Even clinicians and nurses exposed to tragedy can find themselves stuck in this loop.
- Treatment isn’t about pretending risk is zero; it’s about regaining a working relationship with uncertainty so that lifework, family, and rest can restart.
Compulsions that Keep the Cycle Alive
- Endless googling and forum reading
- Asking friends to examine a mole or feel a lymph node
- ER “rule-outs” for the same concern
- Avoiding hospitals, news, or movies that mention disease
- “Magical thinking”: believing a headline or show is an omen that something bad is coming.
End the “Dr. Google” Cycle with CPG
Endless searching won’t bring peace; structured guidance will. Learn how to separate real risk from worry through CBT and practical exposure work.
Health Anxiety vs. Specific Phobias (and other anxiety disorders)
Specific phobias are intense fears of particular objects or situations (needles, flying, heights). With health anxiety, the focus is on being ill or becoming ill, often shifting across conditions (cancer this month, a neurological disease the next) despite normal evaluations.
- What is a specific phobia? A marked fear with immediate anxiety on exposure, avoidance, and distress that isn’t better explained by another disorder.
- DSM-5 criteria for specific phobia include persistent fear (≥6 months), active avoidance, and significant impairment.
- Examples of a specific phobia: blood-injection-injury type, animal type, situational type (flying), natural-environment type.
- Specific phobia ICD-10 / DSM-5 code: typically F40.2x (specifiers by type).
- Prevalence of specific phobia: among the most common anxiety disorders.
- Panic disorder vs. specific phobia: panic disorder features unexpected attacks and worry about future attacks; phobias trigger panic in circumscribed situations.
- Health anxiety vs. Social Anxiety Disorder: social anxiety centers on fear of scrutiny or embarrassment; health anxiety centers on disease and bodily sensations.
While anxiety disorders, specific phobias, and illness anxiety are distinct in their nature, they can co-occur. A person might have a specific phobia of needles and health anxiety about cancer; each requires targeted treatment.
How Clinicians Diagnose it (DSM-5; what to expect)
A primary-care exam rules out urgent medical problems and sets sensible limits on repeat testing. If health worries persist ≥6 months (not necessarily about one illness), with minimal or no symptoms, and cause impairment, clinicians consider illness anxiety disorder.
You may be referred for a structured mental-health evaluation. Questionnaires can help, but diagnosis rests on history, behavior patterns, and functional impact.
It’s also common to review overlap with somatic symptom disorder (more focus on the burden of symptoms) and to screen for GAD, OCD, depression, or substance use that may worsen anxiety.
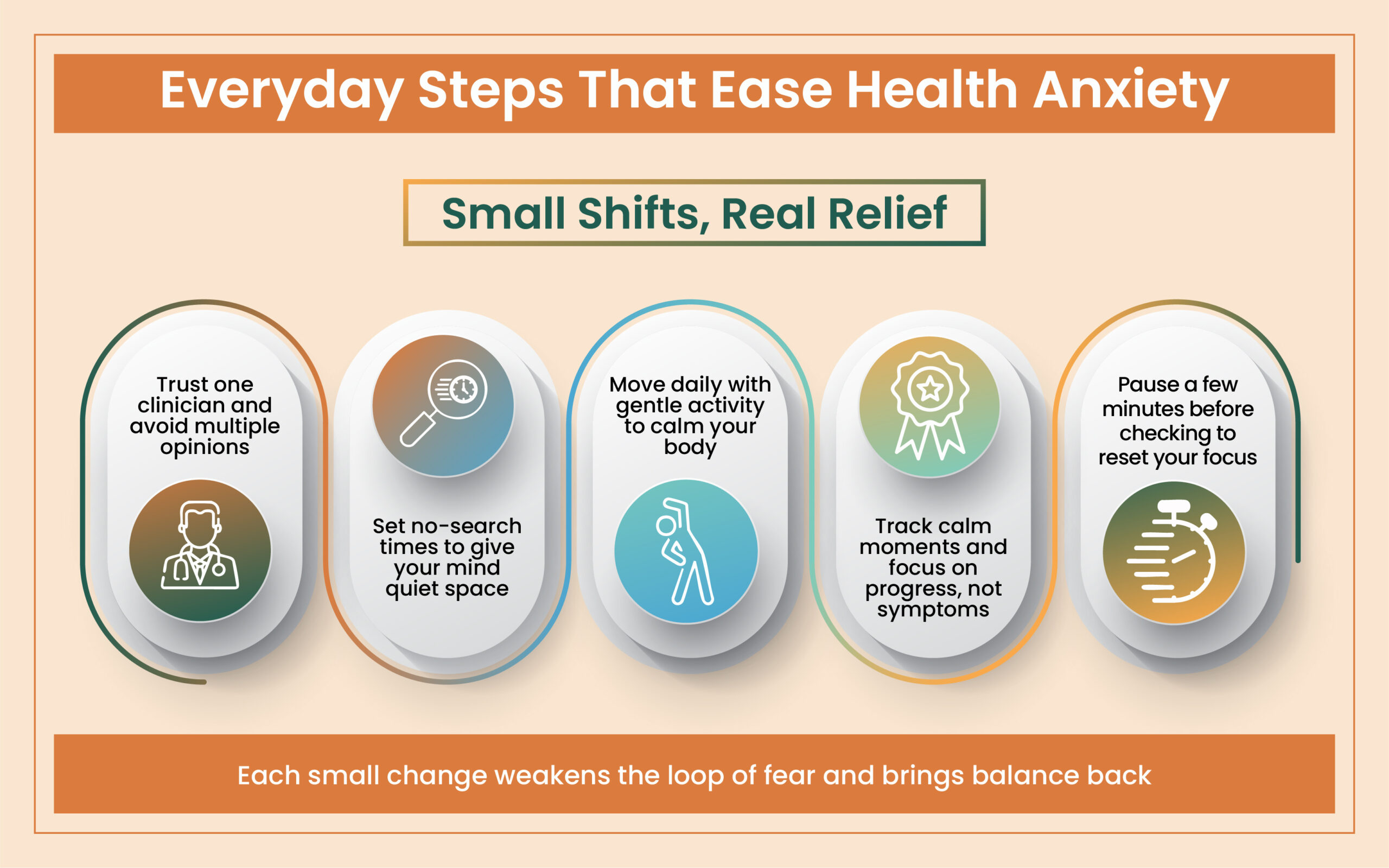
Practical Guide: Small Steps to Manage Health Anxiety
| Challenge You Face | What to Try Instead | Why It Helps |
|---|---|---|
| Frequent Googling for Symptoms | Set a “no-search window” after 8 PM | Reduces constant scanning and unwinding before sleep |
| Repeating Doctor Visits | Choose one trusted clinician | Builds trust and ends the reassurance cycle |
| Anxious when Sensations Appear | Pause, breathe slowly (inhale 4–hold 4–exhale 4) | Remember, sensations aren’t emergencies. Keep your CALM |
| Avoiding activities of “just in case” | Start small — short walk, brief trip, or gentle workout | Rebuilds confidence and helps to relearn safety |
| Seeking reassurance from loved ones | Ask for emotional support (“please listen”) but skip reassurance | Keeps connections strong without feeding the anxiety loop |
What Actually Helps: CBT, Exposure, Medication, and Self-Care
Cognitive Behavioral Therapy (CBT) is the first-line treatment with the strongest durability:
- Psychoeducation: how anxiety magnifies benign sensations and why reassurance backfires.
- Cognitive Redirection: focusing on harmful thoughts; focusing on more balanced responses.
- Exposure with response prevention (ERP): gradually learning to face feared cues (sensations, medical topics, hospitals) while stopping, checking, and reassurance.
- Relapse-prevention: a written plan to keep practice going and catch early warning signs.
Expert Insight
- Many patients describe health anxiety as a “loop that never stops.”
- They check a symptom, feel momentary calm, then the doubt returns stronger.
- Recovery isn’t about proving you’re healthy; it’s about teaching your brain that uncertainty isn’t danger.
- Over time, calm becomes the default, not the exception.
Self-Care Routines that Support Treatment
- Plan brief, regular check-ins with one clinician; avoid doctor-hopping.
- Set guardrails for symptom searching; practice “no-Google windows.”
- Lock in a sleep rhythm; exercise regularly; limit alcohol and cannabis.
- Use mindfulness, paced breathing, or progressive muscle relaxation to settle spikes.
- Return to avoided activities in small steps (workouts, overnights, travel).
- Track “urges to check,” and gradually reduce frequency week by week.
Patterns of Reassurance, Checking, Avoidance, & “Dr. Google”
Reassurance helps for minutes or hours, then the doubt returns: Maybe they missed something. That doubt pushes more searching and checking, which heightens body awareness, which re-inflames fear. Avoidance (skipping clinics, health shows) can bring short-term relief, but keeps the fear intact.
Therapy breaks the loop. A typical ladder might start with reading a balanced article about a feared illness, then watching a short patient story, then walking past a clinic, then scheduling routine care, all while delaying checks and reassurance. Over time, the body learns: “I can feel this discomfort and still live my life”.
Break the Fear–Reassurance Loop
You don’t need to “stop worrying”, you need tools that make worry lose its grip. CPG therapists help you rebuild comfort with your body, one step at a time.
How Loved Ones Can Support without Feeding the Cycle
- Validate feelings, not fears. “I can see how scared this makes you.”
- Limit reassurance. Answer once, kindly, and then redirect to a coping step.
- Encourage treatment. Offer to help schedule an evaluation or sit in on the first telehealth visit.
- Model balanced behavior. Keep normal routines; avoid joining endless online searches.
When to Seek Care & How Online Treatment Works
Seek help if health worries are crowding out work, sleep, or relationships, or if self-help steps haven’t moved the needle. If you or someone you love has thoughts of self-harm, call or text 988 for immediate support.
Capital Psychiatry Group (CPG) provides online/in-clinic mental-health care across New Jersey with same-day appointments. Our psychologists and psychiatrists deliver CBT with exposure, medication management when indicated, and practical plans that fit your life.
Secure video visits include evaluation, goal-setting, stepwise exposures, and coaching on sleep, movement, and digital boundaries. Book a same-day telepsychiatry appointment. CPG serves adults and teens statewide in NJ. Online/in-person with all insurances accepted.
Learn to Trust Your Body Again with CPG
You’ve checked every symptom, now it’s time to check in with yourself. Our online/in-person therapists specialize in health anxiety and help you retrain your response to fear.
Frequently Asked Questions
What’s the difference between illness anxiety and somatic symptom disorder?
Both involve distress about health. Illness anxiety focuses on fear of disease with few or mild symptoms; somatic symptom disorder emphasizes the burden of symptoms themselves. Either can coexist with depression or other anxiety disorders.
What’s the ICD-10 code used for?
Clinicians commonly use F45.21 (Illness anxiety disorder) or related codes depending on presentation. Specific phobia ICD-10 codes fall under F40.2x.
How common is illness anxiety?
Estimates vary widely by setting. Rates rise in primary care and among people living with chronic medical conditions. Many cases go undiagnosed because reassurance temporarily quiets worry.
What’s the DSM-5 criteria snapshot for illness anxiety?
Persistent (≥6 months) preoccupation with serious illness, minimal symptoms, high health anxiety, frequent health-related behaviors (or avoidance), and impairment, not better explained by another disorder.
How we reviewed this article:
CPG experts follow strict sourcing standards, using peer-reviewed research, academic institutions, and trusted medical journals. Only reliable, evidence-based sources are cited to maintain accuracy and integrity.
- https://www.mayoclinic.org/diseases-conditions/illness-anxiety-disorder/symptoms-causes/syc-20373782
- https://my.clevelandclinic.org/health/diseases/9886-illness-anxiety-disorder-hypochondria-hypochondriasis
- https://www.aacn.org/blog/the-journey-to-joy-my-struggles-with-health-anxiety-obsessive-compulsive-disorder
- https://www.healthline.com/health/anxiety/somatic-anxiety
- https://rogersbh.org/blog/10-common-health-anxiety-symptoms/
Our Review Standards
Our team regularly reviews health and wellness writings. Updates are made on the availability of new & authentic information.
Our Editorial Team
Clinical Adviser:
Author:



