
As winter arrives, days become shorter, and as sunlight reduces, silence becomes too heavy to bear. Many people notice these seasonal changes as their energy fades, with feelings of hopelessness, lack of motivation, and more. Some people feel them deeply, and for them, this seasonal change is more than “winter blues.”
This condition or experience, as seasons change, is a form of depression known as Seasonal Affective Disorder (SAD).
In this read, we will study the symptoms, causes (pathophysiology/theories), treatment options, and lifestyle changes that can help you cope with SAD. The mental health experts of Capital Psychiatry Group will also share preventive & seasonal strategies.
Did You Know?
- In the U.S., SAD prevalence ranges from 1.4% in Florida (warm state) to 9.7% in New Hampshire (a cold state).
- About 50–70% experience another SAD episode next winter.
- Global pooled prevalence of SAD is 5.01%.
- Women are about 4 times more likely than men to be diagnosed with SAD.
- SAD usually begins in young adulthood, most often between ages 18 and 30.
SAD Symptoms & What It Feels Like
The winter-onset subtype is far more common, but some people do experience a summer pattern of seasonal affective disorder.
Typical & Atypical Symptoms in Winter-Onset of SAD
In the winter pattern of SAD, the classic “winter blues” can turn clinical. Many patients display atypical depressive features. (there are many similarities between SAD & persistent depressive disorder (excluding the seasonal element)
- Hypersomnia (sleeping longer than usual) or difficulty waking
- Increased appetite, especially cravings for carbohydrates or sweets
- Weight gain
- Low energy, fatigue, heaviness in limbs (often described as “leaden paralysis”)
- Social withdrawal or a reduction of interest in social activities that were previously enjoyed
- Difficulty concentrating, slowed thinking
- Feelings of sadness, hopelessness, guilt
- Lack of motivation, sluggishness
Not sure if it’s SAD or something else?
Understanding the difference between everyday mood shifts and Seasonal Affective Disorder with Capital Psychiatry Group. Our professional evaluation will help clear the confusion.
Summer-Onset (Reverse SAD) Symptoms
The summer SAD, also called reverse SAD, is less common. It appears in spring or summer. The symptoms here are mirrors or opposites of what one might experience in the winter subtype:
- Insomnia or reduced sleep
- Poor appetite, weight loss
- Agitation, restlessness, anxiety
- Irritability rather than lethargy
- Difficulty handling heat or sunlight
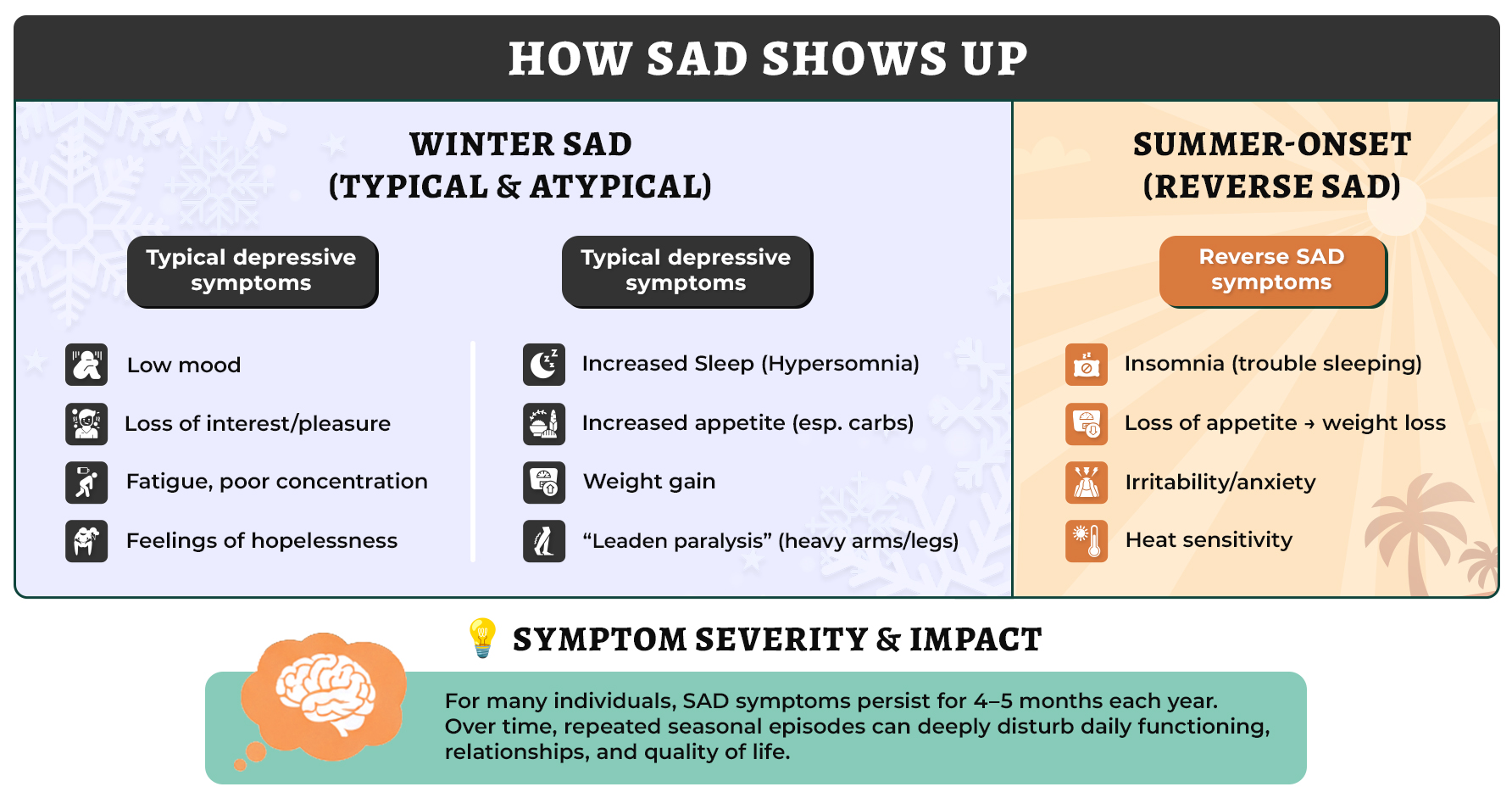
In one early study, concluded that individuals with summer SAD report a decrease in appetite and insomnia rather than an increase in eating habits and sleeping.
Intensity, Duration & Red Flags
- For many individuals, the SAD symptoms last for 4 to 5 months.
- If the severity of symptoms deeply disturbs daily life or causes suicidal thoughts, then it will be classified as a major depressive episode.
Why Does SAD Happen? (Pathophysiology & Theories)
The question “Why do I feel blue in winter?” has always been a question of research. But there is no single or simple answer to this question. The cause of SAD is related to the complex interaction of circadian disruption, neurotransmitter shifts, light sensitivity, and more. Below, we will share the deeper, evidence-based insights for a better understanding.
1. Circadian Rhythm Misalignment (Phase Shift Hypothesis)
There is a small region of the brain called the suprachiasmatic nucleus whose function is to sync the 24-hour light-dark cycle. It acts as the body’s master clock. In SAD, due to reduced sunlight, the phase of this clock is delayed. In the winter, due to less light, your body’s biological signals (melatonin onset, sleep drive, body temperature) occur later than they should.
A recent 2023 wearable-based longitudinal study found that higher depression scores correlate with delayed and irregular circadian rhythms, especially in winter months.
2. Serotonin & Neurotransmitter Regulation
Cerebral serotonin is a key mood-regulating neurotransmitter in our brain, which fluctuates with the seasons. Studies show that in winter, there are more transporters open for binding in the brain. Meaning more serotonin is taken back up (reabsorbed) into nerve cells. As a result, there’s less serotonin available to boost your mood. This may help explain why mood often declines during colder months.
Do seasons keep changing how you feel?
You don’t have to wait for spring to feel better. With the right support from CPG, you can manage your symptoms and stop this depressing cycle from coming next year.
3. Melatonin & Darkness Response
Melatonin is the hormone in your body that is released in the dark. It is the body’s natural alarm for nighttime as it prepares your body for sleep. In SAD, melatonin secretion may become prolonged (last longer) during longer winter nights. This usual increase in melatonin during winter darkness has stronger mood and sleep effects.
4. Reduced Light & Photoperiod Sensitivity
This shorter photoperiod (fewer daylight hours) increased the depressive symptoms in people with SAD.
The photon-count hypothesis research indicates that during winter, fewer daylight photons reach the retina than in summer. This reduction of light isn’t enough for the brain’s mood circuits to regulate properly.
5. Genetic / Vulnerability & Behavioral Modulators
- Biological factors do not develop or function in the same way for everyone. Some individuals carry variants in circadian clock genes (such as PER3 and NPAS2) that regulate the body’s internal 24-hour clock. Or the serotonin transporter gene (5-HTTLPR) that is crucial for mood regulation. These genes can increase small-to-moderate amounts of risk of SAD.
- In winter, there are fewer outdoor activities than in summer. Therefore, people move less, don’t socialize as much like the summer. Plus, reduction of sunlight also means lower vitamin D. All of these factors can increase the biological vulnerability and may contribute to symptoms of SAD.
How SAD Is Diagnosed & Assessed
The able psychologists and psychologists of Capital Psychiatry Group accurately diagnose with the help of structured evaluation, validated tools, and clinical judgment via state-wide clinics and HIPAA-secure telehealth. We distinguish SAD from other mood conditions to provide a personalized treatment plan online.
DSM Specifier: “With Seasonal Pattern”
SAD is not a standalone recognized mental health disorder in DSM-5 (or DSM-5-TR). Rather, it’s a specifier added onto diagnoses such as Major Depressive Disorder (MDD) or Bipolar Disorder.
To apply the “with seasonal pattern” specifier correctly, our board-certified clinicians look for:
- There should be a regular temporal relationship between the onset of major depressive episodes or bipolar mood episodes during a particular season (e.g., fall/winter).
- As the reason goes by, there should be full remission or reduction of severity of symptoms (e.g, depressive symptoms vanish in the spring).
- Across the past two years, episodes follow the same season, with no non-seasonal episodes in that interval.
- During the person’s lifetime, the mood changes with a seasonal pattern should outnumber the non-seasonal episodes.
If a patient meets the full criteria for MDD or Bipolar Disorder, and this seasonal pattern, then the diagnosis may be recorded as “MDD, recurrent, with seasonal pattern.
Do shorter days drain your mood?
If every winter starts with a heavy feeling and is harder to get through, it can be more than seasonal changes. Capital Psychiatry Group helps you cope when the symptoms start to disturb your daily life.
ICD-10: No Official “SAD” Code
In ICD-10, there is no specific code for SAD. Instead, SAD is applied to mood (affective) disorders, categories F30-33.
- A person must have at least three mood episodes (e.g., depressive episodes) for three consecutive years. The episode should always begin within a 90-day seasonal window.
- The depressive episode symptoms must also lose severity during the next season each year (e.g, spring) for a consistent 90 days.
- For diagnosis, the seasonal episodes must outnumber other depressive episodes that happen during the non-seasonal times.
The 90-day seasonal window criteria are for research proposals, not an official ICD-10 requirement.
Seasonal Pattern Assessment Questionnaire (SPAQ)
SPAQ was developed by Rosenthal and colleagues in 1984. To this day, it remains the most widely used screening tool for seasonal mood variation.
In these questionnaires, mental health experts ask individuals to rate their mood, sleep, appetite, weight, social activity, and energy according to the seasons.
If the “seasonality score” is higher than it may suggest clinically significant seasonal effects.
Some studies indicate SPAQ may overestimate seasonal patterns, i.e., false positives. Therefore, it is used as a screening tool, not as a final diagnostic tool.
Seasonal Affective Disorder Treatments & Therapies
Seasonal affective disorder therapies and anti-depression medication are the most effective treatment options for SAD. Lifestyle strategies are important adjuncts. In care at Capital Psychiatry Group, our HIPAA-compliant in-clinic and telehelp combines all of these options based on your symptoms and preferences.
1) Bright Light Therapy (BLT)
In BLT, individuals sit near a 10,000-lux light box for around 30 minutes each morning. Eyes should be open but not staring straight into the light. This treatment option corrects the circadian “phase delay” common in SAD.
Wondering if Bright Light Therapy (BLT) will work for SAD?
Our professionals will guide you to get the right help. Book a personalized session and receive help from industry-leading psychologists and experts at CPG.
2) Antidepressant Medication
Note: This is not medical advice and is not equivalent to the doctor’s observation.
- SSRIs (Selective Serotonin Reuptake Inhibitors)
Common SSRIs such as fluoxetine (Prozac) and sertraline (Zoloft) have been proven to be effective for the treatment of winter depression. In 2021, a review by Cochrane found that fluoxetine is almost as effective as light therapy in reducing acute SAD symptoms. - Bupropion XL (Extended-Release)
Bupropion XL is the only medication that has been proven to prevent SAD from coming back each winter. It is also the only FDA-approved drug specifically for SAD. When this medication is used at the start of fall/winter, it reduces the risk of a depressive episode. Moreover, in 2019, a large analysis of over 1,000 patients found that bupropion cut the chance of recurrence by nearly half compared to placebo.
Side-effects & cautions
Some side effects of seasonal affective disorder medication are headache, insomnia, and nausea.
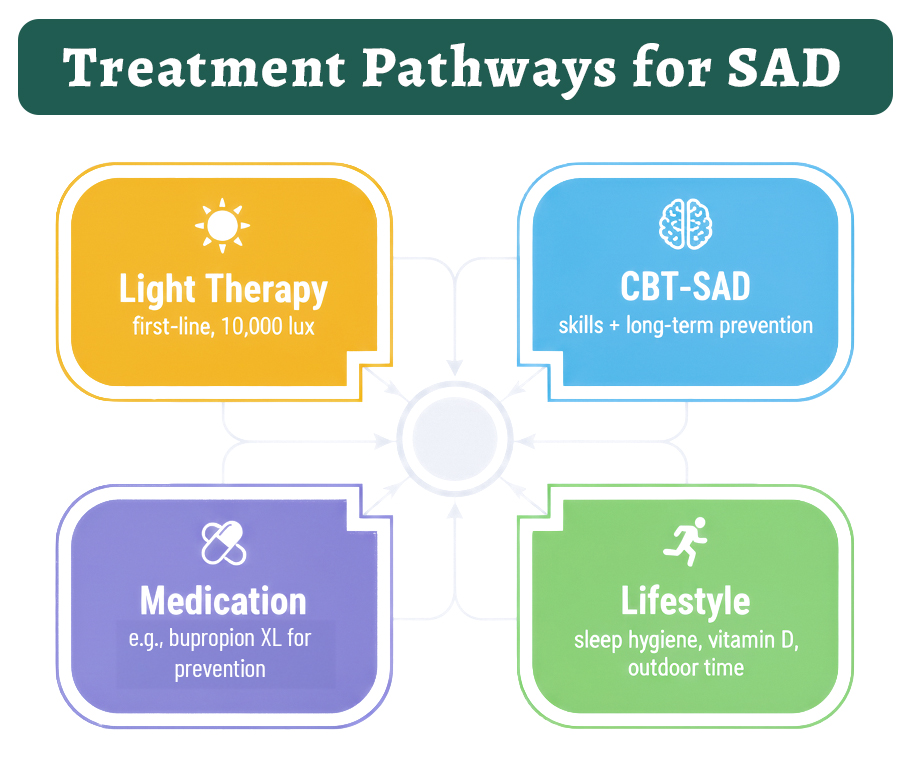
3) Cognitive Behavioral Therapy for SAD
CBT is a structured, skills-based therapy and is often called the gold standard of therapy. For Seasonal Affective Disorder, it has been adapted into CBT-SAD, a program that combines behavioral activation and cognitive reframing.
Behavioral activation processes energize and help create healthy routines in winter that avoid withdrawal and inactivity.
Cognitive reframing identifies the depressing seasonal thoughts, such as I can’t function in winter and reshapes them into more balanced, realistic perspectives.
It basically helps you adapt better routines and change negative thoughts into good ones. CBT-SAD and BLT, when combined, are the most effective treatments for SAD. It improves engagement and day-to-day functioning while symptoms diminish.
Expert Insight
In a head-to-head trial, CBT-SAD and light therapy were equally effective. But CBT-SAD had fewer recurrences two winters later (27.3% vs. 45.6%). This durability makes CBT-SAD a strong option to prevent relapse.
4) Self-Care, Lifestyle & Preventive Strategies
You can handle the symptoms with self-care by structuring daylight, sleep, movement, and nutrition around your biology. These preventive measures and lifestyle changes won’t replace treatment for moderate or severe seasonal affective disorder, but they help you manage symptoms and prevent relapse.
- Consistent morning light exposure
- Lock in a winter sleep rhythm
- Exercise and increase daytime outdoor time
- Check Vitamin D levels and treat deficiency
Why Choose Us for Seasonal Affective Disorder Care
Every person experiences Seasonal Affective Disorder (SAD) differently. Capital Psychiatry Group understands how symptoms and their severity are different for everyone. Therefore, we focus on precise evaluation and deliver evidence-based treatment.
- All insurances accepted
- Same-day, weekend & walk-in appointments
- Board-certified psychiatrists & psychologists
- HIPAA-compliant telepsychiatry
- In-clinic care across New Jersey
- Personalized and evidence-based plans
- Online & in-person appointments
- Ongoing support & follow-up
Takeaway
Seasonal Affective Disorder is more problematic than “winter blues”. Its symptoms often last for 4 to 5 months and may return annually in the same time of season. It can show up in the form of winter fatigue, summer insomnia, or low energy. Over time, these repeated seasonal episodes deeply disturb daily functioning and overall quality of life.
The good news is that SAD is treatable with some evidence-based FDA-approved medication and light therapy, and CBT-SAD. All of them, when combined, provide effective ways to ease symptoms and prevent recurrence.
Losing Energy Every Winter?
If every winter feels heavier and depressing, it could be more than seasonal changes. Learn what your symptoms really mean through our board-certified providers via telepsychiatry.
How we reviewed this article:
CPG experts follow strict sourcing standards, using peer-reviewed research, academic institutions, and trusted medical journals. Only reliable, evidence-based sources are cited to maintain accuracy and integrity.
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3004726/
- https://www.ncbi.nlm.nih.gov/books/NBK568745/
- https://emedicine.medscape.com/article/2500054-overview
- https://www.sciencedirect.com/science/article/abs/pii/S0165032725012492
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10741218/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4673349/
- https://pubmed.ncbi.nlm.nih.gov/1791262/
- https://arxiv.org/abs/2312.02953
- https://research.regionh.dk/en/publications/patients-with-seasonal-affective-disorder-show-seasonal-fluctuati
- https://www.cambridge.org/core/services/aop-cambridge-core/content/view/83DE1192351D19A4E50177A41FE9A9A1/S1355514600015212a.pdf/seasonal-affective-disorder.pdf
- https://www.sciencedirect.com/science/article/abs/pii/S0022395625002985
- https://www.nimh.nih.gov/health/publications/seasonal-affective-disorder
- https://www.psychiatry.org/patients-families/seasonal-affective-disorder
- https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008591.pub3/full
- https://academic.oup.com/book/24578/chapter-abstract/187837936
- https://pubmed.ncbi.nlm.nih.gov/30883669/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5797481/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3652773/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4939843/
- https://www.health.harvard.edu/blog/light-therapy-not-just-for-seasonal-depression-202210282840
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4141118/
Our Review Standards
Our team regularly reviews health and wellness writings. Updates are made on the availability of new & authentic information.
Our Editorial Team
Clinical Adviser:
Author:



