
What is Cognitive Behavioral Therapy?
How and What of CBT
- “I’m going to panic,”
- “They think I’m weird,”
- “Nothing ever changes.”
Turn Racing Thoughts Into Action
Restructuring and Behavioral Activation Via Therapy
- What you think about a situation affects how you feel and what you do.
- Some of those thoughts are distorted, automatic, or overly negative.
- When you change those thoughts and the behaviors that follow, symptoms often ease, and daily life becomes more workable.
Expert Insights: Making CBT Work in Everyday Life
- CBT works best when the therapy room isn’t the only place you use it.
- The patients who get the most out of cognitive behavioral therapy for anxiety, depression, OCD, or insomnia are not the ones who never struggle; they’re the ones who practice tiny skills on tough days.
- That might mean doing a two-minute thought record after a spike of panic, sticking to a sleep window even when you’re tempted to nap, or taking one exposure step toward a feared situation instead of avoiding it altogether.
- At Capital Psychiatry Group, therapists keep CBT realistic. You won’t be sent home with a stack of worksheets you’ll never touch.
- Instead, you work together to design doable CBT exercises that fit your schedule and energy level:
- One breathing drill to use in meetings.
- One social interaction to try this week.
- One small behavioral activation task when depression is heavy.
- Over time, those “small” changes rewired into your day are what shift chronic patterns like rumination,
CBT is widely used as a First-line Treatment
- Depression and major depressive disorder
- Generalized anxiety disorder, panic attacks, and social anxiety
- OCD and intrusive thoughts
- PTSD and trauma-related symptoms
- Insomnia and sleep anxiety (CBT-I)
- ADHD, executive dysfunction, and procrastination
- Phobias and agoraphobia
- Bipolar disorder and schizophrenia (alongside medication)
- Chronic pain, IBS, migraines, and other stress-sensitive conditions
Sleep Better With CBT-I
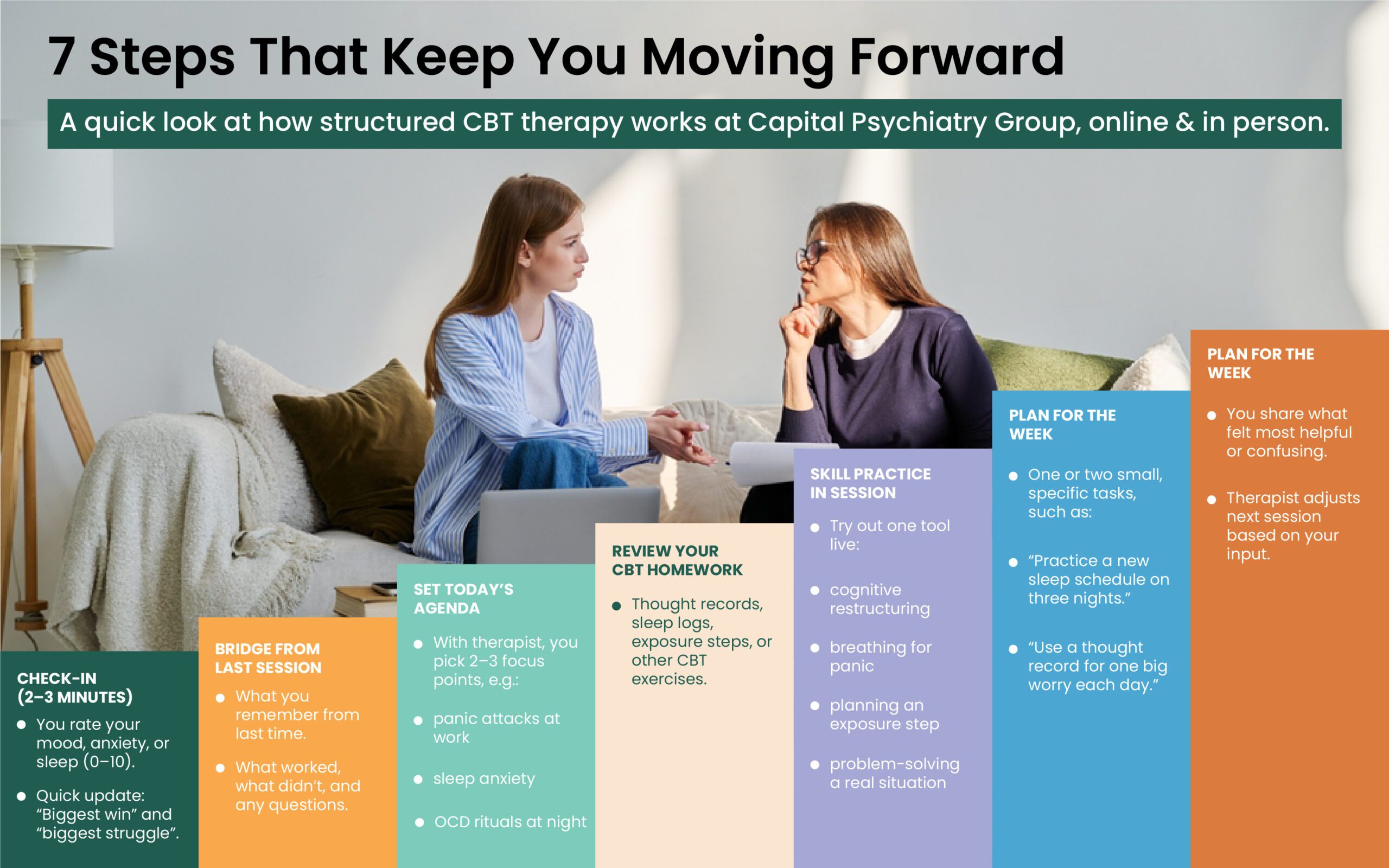
How CBT Works: Step-by-Step Process
1. Assessment and Goal-setting
You and your therapist identify:
- What’s bothering you (for example: “constant worry,” “panic in stores,” “rumination at night”)
- How these problems show up: thoughts, feelings, and behaviors
- What you want to change (sleep better, reduce panic, stop avoiding, feel less depressed)
Together, you turn this into specific, realistic CBT goals, not just “feel better,” but things like:
- “Cut panic attacks from 4 per week to 1 or none.”
- “Fall asleep within 30 minutes most nights”.
- “Return to work or school three days a week”.
2. Collaborative Case Formulation
Your therapist helps you map out how things currently work for you:
- Triggers/situations (crowded stores, conflict with a partner, being alone, physical sensations)
- Automatic thoughts (“I’m not safe,” “I’ll be abandoned,” “This will never get better”)
- Emotions and body reactions (fear, shame, tight chest, dizziness, muscle tension)
- Behaviors (avoidance, reassurance seeking, anger outbursts, compulsions, substance use, scrolling late into the night)
3. Core CBT Techniques in Practice
- Cognitive restructuring: categorizing distorted thoughts and challenging them against the facts, and providing more balanced alternatives.
- Behavioral activation: Gradually re-introducing meaningful activities, movement, social contact, hobbies, and self-care when low mood or fatigue is prevalent.
- Exposure therapy: Carefully planned, step-by-step practice facing the situations or sensations you usually avoid (crowds, driving, social events, bodily sensations), especially in CBT for panic disorder, social phobia, PTSD, and OCD.
- Skills for emotion regulation: Breathing, grounding, problem-solving, and communication skills to help with anger, shame, or feeling overwhelmed.
- Sleep and routine work: For cognitive behavioral therapy for insomnia and sleep anxiety, you’ll adjust sleep schedules, wind-down routines, and unhelpful “sleep rules” that keep you wired at night.
CBT Support For Anxiety & Depression
Measuring Progress and Planning Next Steps
What CBT Helps with: Symptoms and Conditions
Cognitive Behavioral Therapy for Anxiety
Cognitive Behavioral Therapy for Depression
CBT for OCD and Intrusive Thoughts
CBT for PTSD and Trauma
CBT for insomnia (CBT-I)
CBT for ADHD and Executive Dysfunction
CBT for Kids and Teens
Specialized CBT For OCD & Trauma
Main Types of CBT you might Encounter
- “CBT” is an umbrella. Under it are several related approaches, often chosen based on your main symptoms:
Standard CBT (Beck-style cognitive therapy)
The foundation: structured sessions, thought records, cognitive restructuring, and behavior change. - Exposure-based CBT
Gradual “practice” facing feared situations or sensations, for phobias, panic disorder, agoraphobia, social anxiety, OCD, health anxiety, and trauma cues. - Trauma-focused CBT
Combines CBT tools with structured trauma processing for PTSD, complex trauma, and some grief reactions. - Mindfulness-based CBT (MBCT)
Merges CBT with mindfulness training to break cycles of depression and chronic worry by helping you notice thoughts without getting pulled in. - Acceptance and commitment–based CBT (ACT)
Emphasizes accepting internal experiences, clarifying your values, and taking committed action even when anxiety, intrusive thoughts, or pain are present. - CBT-I (for insomnia)
A specialized protocol for sleep anxiety and chronic insomnia, reshaping both sleep habits and sleep-related thinking. - CBT for psychosis and bipolar disorder
Used alongside medication to address paranoia, residual psychotic symptoms, mood swings, and self-stigma, and to catch early warning signs of relapse.
Core CBT techniques and exercises
1. Cognitive restructuring (thought challenging)
- Catch automatic thoughts in real time
- Examine the evidence for and against those thoughts
- Generate more balanced alternatives
2. Behavioral activation
Depression and anxiety often push you to do less. Behavioral activation reverses that:
- You schedule small, doable activities tied to pleasure or a sense of mastery
- You track mood before and after, to see how behavior shifts feelings
- Over time, your day fills with more healthy structure and less isolation
3. Exposure and response prevention
For OCD, phobias, social anxiety, panic, agoraphobia, and trauma reminders, CBT often uses graded exposure:
- Build a fear hierarchy (from mildly uncomfortable to extremely scary)
- Start with the easier items and stay with the feeling instead of escaping or using safety behaviors
- As your nervous system learns you can handle it, the fear response gradually drops
4. Skills training and coping strategies
- Relaxation and breathing techniques for panic and stress
- Problem-solving and decision-making skills
- Communication and assertiveness skills for relationship problems and social anxiety
- Anger and emotional regulation strategies for mood swings, irritability, or outbursts
5. Homework and CBT exercises at home
A key feature of CBT, and of brief CBT manuals, is practice between sessions. Common assignments include
- Keeping a thought or worry log
- Filling out thought records when distress spikes
- Doing planned behavioral experiments (for example, “I will attend one social event without safety behaviors and see what actually happens”)
- Practicing a sleep schedule for CBT-I
- Working through specific CBT exercises for intrusive thoughts, panic, or trauma cues
Expert Insight: Why CBT Matters Alongside Medication
- Many people arrive in CBT treatment already taking medication for anxiety, depression, bipolar disorder, or PTSD and still feel stuck.
- Medication can calm the volume of symptoms, but it can’t, by itself, teach you:
- How to stop checking the door ten times?
How to face crowded spaces again, or how to challenge?
the “I’m a failure” story that has followed you for years. - That’s where cognitive behavioral therapy treatments add something medication simply can’t provide.
- In our psychological services at CPG, CBT and medication management are often paired deliberately.
- Medication may create enough stability that you can fully engage in exposure therapy for OCD, cognitive behavioral therapy for panic disorder, or CBT for trauma and stress disorders.
- CBT then focuses on the patterns that keep symptoms alive, negative thinking, safety behaviors, sleep habits, and avoidance.
- The goal isn’t to choose medication or therapy, but to build a plan where each supports the other so you’re not just surviving, you’re actively rebuilding how you think, feel, and live
What to expect in CBT with Capital Psychiatry Group
- Format: 45–50 minute sessions, usually weekly at first, then spaced out as symptoms improve. Available in-person and via telepsychiatry/teletherapy.
- Length of treatment: Many brief CBT plans run 8–20 sessions, depending on the complexity and severity of symptoms. Some people continue longer for relapse prevention or additional goals.
- Integration with medication management: Your CBT therapist may coordinate with your medication management provider for conditions like bipolar disorder, schizophrenia, severe OCD, or major depressive disorder.
- A focused discussion of current symptoms and history
- Clarifying what you want to change
- An explanation of how CBT works and what your role is
- Agreement on first goals and, often, a very small piece of homework
Final Words
Flexible Care: In-Office Or Online
Quick Q&A about CBT
Do CPG Accept Insurance?
How long does CBT therapy take?
Is CBT effective for PTSD, OCD, and panic?
CBT vs DBT: which is better?
Can CBT be done online?
How we reviewed this article:
- https://www.mayoclinic.org/tests-procedures/cognitive-behavioral-therapy/about/pac-20384610
- https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10440210/
- https://medicine.umich.edu/sites/default/files/content/downloads/Behavioral-Activation-for-Depression.pdf
- https://reachbh.org/what-principle-underlies-cognitive-behavioral-therapy/
- https://www.recoveryanswers.org/resource/cognitive-behavioral-therapy-approaches/
- https://cares.beckinstitute.org/about-cbt/
- https://my.clevelandclinic.org/health/treatments/acceptance-and-commitment-therapy-act-therapy
- https://my.clevelandclinic.org/health/treatments/25067-exposure-therapy
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4396183/
- https://pubmed.ncbi.nlm.nih.gov/22340145/
- https://my.clevelandclinic.org/health/treatments/acceptance-and-commitment-therapy-act-therapy
- https://www.veteranshealthlibrary.va.gov/142,41434_VA
Our Review Standards
Clinical Adviser:
Author:



