
Contamination OCD is not a preference for cleanliness, contrary to what people sometimes oversimplify. It’s a pattern in which intrusive fears of contamination, by germs, illness, chemicals, “impurity,” or even names and images, ignite intense anxiety.
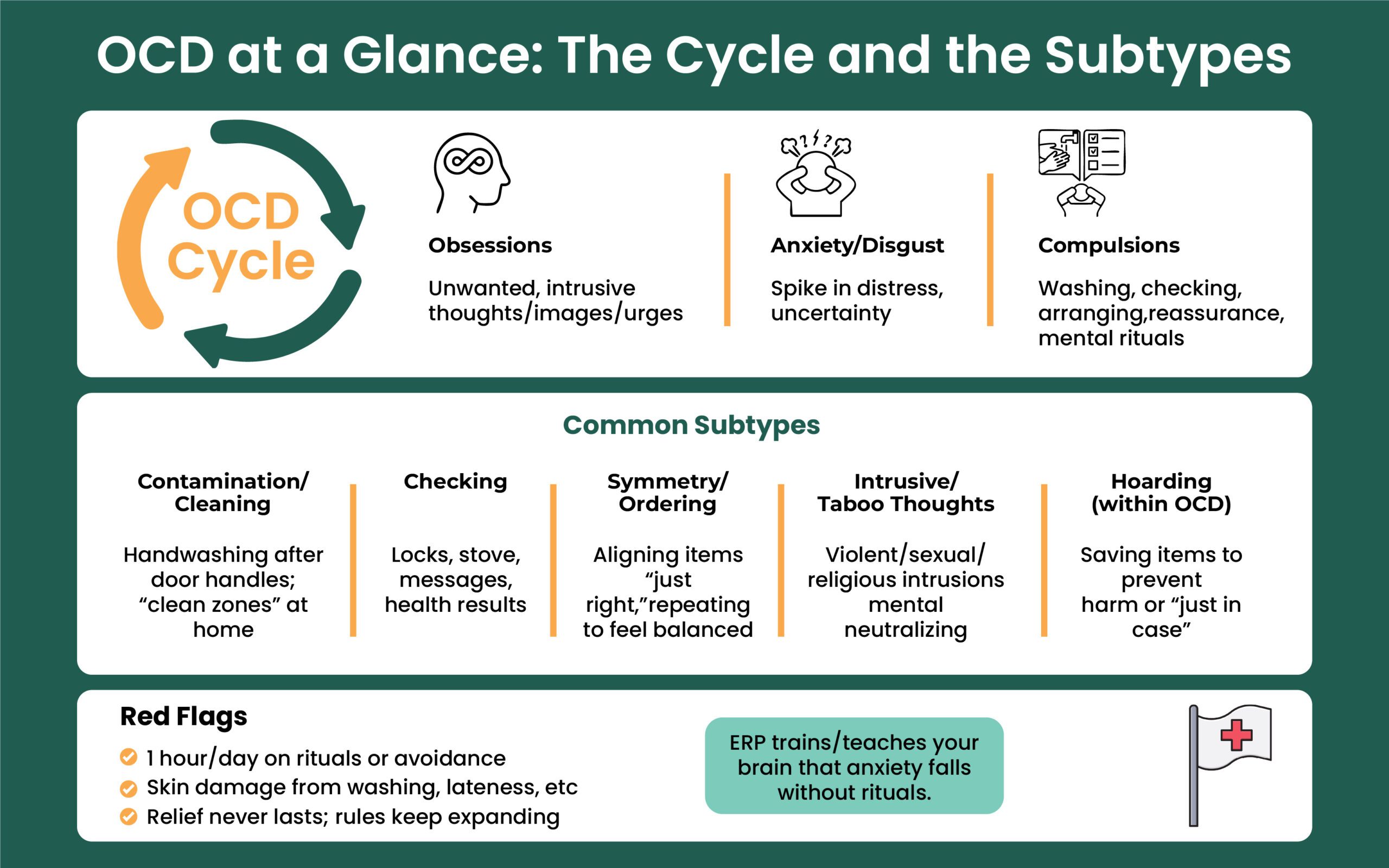
It will also instill habits into rituals such as washing, disinfecting, avoiding, checking, and mental “neutralizing.” Relief is brief, and the cycle restarts. This is different from being careful during flu season: the thoughts are unwanted and sticky, the distress is high, and the rituals are time-consuming and life-limiting (obsessions → anxiety → compulsions → short relief → more obsessions).
Deep Dive into Types of Contamination OCD
- “Clean vs. dirty worlds”: some people maintain separate zones (even separate cars) that must never “touch.”
- Hyper-responsibility subtype: fear of spreading contamination to others and living with guilt.
- Mental/emotional contamination: “taint” transferred by thoughts, names, images, places, or ‘toxic’ people even without touch.
- Law of contagion staying power: the belief that contamination persists across multiple degrees of contact.
- Disgust × obsessive beliefs model: contamination fear intensifies when high disgust propensity combines with beliefs like overestimation of threat and intolerance of uncertainty; disgust can extinguish more slowly than fear.
What Counts as “Contamination” in OCD?
A common belief is that a tiny amount of a contaminant spreads endlessly (e.g., “one drop could taint the whole room”). Many people split life into clean vs. dirty zones, even designating “clean cars” and “dirty cars”, and keep strict rules so the worlds never meet.
Some focus on hyper-responsibility, fearing they’ll contaminate others and live with the guilt. Contamination in OCD is broad. Alongside dirt, viruses, and bacteria, people may fear:
- Bodily fluids and waste: urine, feces, sweat, saliva, mucus, tears, blood, semen.
- Substances/objects: garbage, sticky residues, spoiled food, household chemicals/cleaners, radioactivity, broken glass, lead, asbestos, newsprint, and even soap.
- Animals and people: pets/birds/dead animals; people who look unwell or “unclean”.
- “Magical” or mental contamination: thoughts, words, names (of illnesses or people), places where bad things happened, colors, “bad luck,” images, believed to “transfer” without physical contact.
- Emotional contamination: fear that a person’s “toxic” traits, negativity, or wrongdoing could cling to you merely by being around them.
Take Back Hours Lost to Rituals
OCD steals time through checking, cleaning, and mental loops. We use ERP and CBT, delivered online in New Jersey, to help you get that time back.
Contamination OCD Symptoms
Most people experience both obsessions and compulsions; one can be subtler than the other.
Obsessions (thoughts, images, urges)
- “What if I get seriously ill from this doorknob?”
- “What if I spread disease to my family?”
- “Even saying the name of an illness could ‘taint’ me.”
- “I’ll never feel clean enough.”
- Law of contagion worries: if something touched something “dirty,” it’s still dangerous many steps later.
- Bodily-waste themes: overwhelming fear of urine/feces traces, humiliation if others “find” it, or never achieving “clean”.
Compulsions (behaviors or mental acts)
- Excessive, ritualized washing/showering: counting or exact sequences; washing until skin is raw.
- Disinfecting/sterilizing, sometimes with harsh agents; throwing items away.
- Separating “contaminated” vs. “safe” items/areas, creating no-entry zones for others.
- Clothes changes, laundering rules; avoiding bathrooms, public places, or people.
- Barriers and workarounds: gloves, paper towels, plastic bags to touch things.
- Reassurance seeking and checking (“Did I get it on me?” “Is this safe?”)
- Mental rituals to “cancel” thoughts (prayers, repeating words, reviewing steps)
Bodily-waste–focused compulsions can dominate time: prolonged wiping (even to bleeding), visually inspecting toilet paper, avoiding washing other body parts after touching “taboo” areas, scanning for brown marks, and mentally tracking what touched what.
Health consequences are common: cracked, bleeding skin; chemical irritation from disinfectants; and nutritional changes if food is avoided.
Common Triggers
Doorknobs, shared remotes/phones, public restrooms or transit, handling money, hospital/clinic settings, raw or prepared foods, shaking hands/hugging, news of outbreaks, moral/religious “impurity” cues, and broad cues like “the floor/outdoors feels dirty.” Triggers also include people or places associated with harm or shame, even without contact.
- People/places triggers (e.g., shabby/unwell people, places where “bad things” happened).
- Names/colors/bad luck as “contaminants.”
- Extreme time-cost examples: washing 50–200 times/day, showers lasting hours; skin damage and even bleach burns from over-cleaning.
- Toilet-specific compulsions: over-wiping to injury, scrutinizing paper, avoiding washing other body parts after touching “taboo” areas.
- Food contamination concerns (prep/eating exposures).
- Differentiation between “germaphobe” vs. contamination OCD (time cost, impairment, compulsions).
Separate Fact from Fear with CPG
Intrusive thoughts aren’t intentions. Learn evidence-based skills to stop reassurance-seeking and reduce compulsions, step by step.
Why does Contamination OCD take Hold?
There isn’t one cause. Several factors converge:
- Biology & learning: genetic vulnerability, brain-circuit differences, and learned avoidance patterns.
- Disgust propensity: a tendency to feel disgust strongly and often, is tightly linked to contamination fear.
- Obsessive beliefs that amplify disgust and anxiety:
- Overestimation of threat (“If it might be dirty, it’s dangerous”)
- Intolerance of uncertainty (“I must be 100% sure it’s safe”)
- Importance/control of thoughts (“Thinking ‘dirty’ makes it real; I must neutralize it”)
- Inflated responsibility & perfectionism (“If anyone gets sick, it’s on me; it must be perfectly clean”)
Research shows disgust + obsessive beliefs interact: when both are elevated, contamination fear and impairment are stronger. Safety behaviors (washing, avoiding, researching, and reassurance) bring short-term relief but preserve fear and keep the cycle running.
Expert Insights : The Reassurance Trap
Answering “Am I safe? Did I contaminate someone?” calms briefly but teaches the brain that doubt is dangerous.
We replace reassurance loops with micro-tolerances: short, timed pauses, no Googling, and values-based re-engagement. Over days, the urge drops on its own.
Diagnosis and What a “Contamination OCD Test” Really Means
There’s no single test; diagnosis is clinical. A professional assesses obsessions/compulsions that take significant time, cause distress, or impair functioning, while ruling out medical causes or substances. Insight varies, from recognizing beliefs are likely untrue to being fully convinced. Severity often fluctuates with stress.
A Plan for Your Specific OCD Type
Contamination, checking, symmetry, taboo thoughts, each need a tailored roadmap. Get a precise plan plus medication management when needed.
Contamination OCD in Children
Kids can show excessive handwashing, cleaning rituals, avoiding “dirty” places/objects, overusing gloves/sanitizers, and distress at school, on playgrounds, or with peers. Intensity can swing with stress (e.g., exams).
Contamination OCD Treatment
First-line: Exposure and Response Prevention (ERP)
ERP is the most supported therapy for OCD. You gradually face triggers (exposure) while refraining from rituals (response prevention). Examples:
- ERP specifics: dissolving “clean zones,” cross-contact exercises, delaying/reducing counts and durations, not doing mental neutralizing, approaching names/places/images for emotional/mental contamination.
- Family/roommate coaching to stop accommodation and reduce reassurance.
- ACT/mindfulness to tolerate disgust, shame, and uncertainty; not a replacement for ERP, but a support.
- Medication options listed explicitly (SSRIs, clomipramine; selective augmentation).
- Higher-level care: Intensive outpatient/residential ERP, TMS (FDA-cleared devices for adult OCD), DBS for rare refractory adult cases.
- Home supports aligned with ERP: urge surfing, delay-and-dilute rituals, drop back-tracing, and online research limits, reassurance boundaries.
- Child-focused ERP with family therapy and school/peer impact notes; PANDAS consideration.
ERP is paced and collaborative. Nothing is sprung on you. Over time, you learn that feared outcomes don’t occur, or are tolerable, and that you can live with normal risk. Family members learn to stop accommodating rituals and to cut reassurance that feeds the cycle.
Cognitive and Mindfulness Supports
- CBT techniques target black-and-white thinking, catastrophizing, and the law of contagion assumptions.
- ACT and mindfulness teach letting thoughts/feelings come and go without compulsions, building tolerance for disgust, shame, and uncertainty.
Expert Insights : ERP Works Because It Targets the Right Link
OCD isn’t overthinking; it’s an over-learning problem. ERP doesn’t argue with the thought; it retrains the brain’s threat system by pairing feared cues with no ritual.
The nervous system updates: “Nothing happened, and I coped.” That’s durable learning.
Medication management for OCD
Medicine can reduce the intensity of obsessions/compulsions and boost ERP work. Frequently used options include SSRIs (fluoxetine, sertraline, fluvoxamine, paroxetine, citalopram/escitalopram) and clomipramine; sometimes clinicians add an augmentation agent if needed. Many people do best with therapy + medication.
Note: This is not medical advice and is not equivalent to the doctor’s observation.
When Symptoms are Severe or Treatment-Resistant
Structured intensive outpatient/residential ERP, TMS (FDA-cleared devices for adult OCD), and DBS for select refractory adult cases are options when standard care isn’t enough.
Care from Home, Results in Life
No waiting rooms. Secure telepsychiatry & onsite care, structured therapy, and follow-ups that fit your schedule, without pausing your routine.
How to Treat Contamination OCD at Home
- Delay and dilute rituals: wait 10 minutes before washing; trim steps/time; skip one checking loop
- Stop the research spiral and set reassurance limits with loved ones
- Urge surfing: notice “wash now” urges without acting on them; allow discomfort to rise/fall
- Drop tracking: abandon contamination logs and back-tracking
- Family reset: reduce accommodations and “cleaning on behalf of” the sufferer, in a planned, graded way
Contamination OCD vs. “Germaphobia” or “Cleanliness OCD”
Germ aversion alone isn’t OCD. Contamination OCD involves intrusive obsessions plus compulsions that consume time and disrupt school, work, relationships, or health. Many with OCD contamination know the rules feel excessive, yet feel driven to follow them “just in case.”
Care with Capital Psychiatry Group
We provide online and in-clinic OCD care, with same-day appointments when available. Treatment plans of Capital Psychiatry Group combine ERP, CBT/ACT, and medication management for OCD. Our Outpatient mental health services coordinate with families, offer child/adolescent services, and support you in merging “clean vs. dirty worlds” so life opens back up.
- Learn more about our approach to OCD and ERP: OCD treatment
- Same-Day & Weekend Appointments Available.
- Serving New Jersey with telepsychiatry and 7+ in-clinic options.
End the “What Ifs” Today with CPG
OCD thrives on doubt. We’ll cut the loop with ERP, practical tools, and when needed, medication management, all online in New Jersey with same-day starts.
FAQs
What are contamination OCD symptoms?
Intrusive fear of germs/fear of contamination, disgust, cleaning rituals, separation of clean vs. dirty items, throwing things away, reassurance seeking, and mental “neutralizing.”
Is there a contamination OCD test?
Screeners can flag patterns, but diagnosis is a clinical evaluation that considers insight, time cost, distress, and impairment.
How to stop contamination OCD at home?
Use ERP-style steps: delay and reduce rituals, limit reassurance, and practice exposures safely. Home strategies support, not replace, professional care.
What is emotional or mental contamination?
Feeling “contaminated” by people, places, names, images, or “bad energy,” even without contact, is treated with the same ERP principles.
Food contamination OCD—what helps?
Graded exposures: cook/eat with reasonable hygiene, avoid re-washing cycles, and stop throwing food out without evidence.
Medication for contamination OCD?
SSRIs or clomipramine; sometimes augmentation. Best outcomes often pair medication management for OCD with ERP.
How we reviewed this article:
CPG experts follow strict sourcing standards, using peer-reviewed research, academic institutions, and trusted medical journals. Only reliable, evidence-based sources are cited to maintain accuracy and integrity.
- https://iocdf.org/expert-opinions/expert-opinion-contamination/
- https://www.treatmyocd.com/blog/contamination-ocd-fear-of-germs
- https://canyoncreekbh.com/blog/what-is-contamination-ocd-causes-symptoms-care/
- https://ocditexas.com/contamination-ocd/
- https://www.handspringhealth.com/post/contamination-ocd
- https://www.ocdanxietycenters.com/ocd/exposure-therapy-for-cleanliness-and-contamination-ocd/
- https://www.cambridge.org/core/books/abs/heuristics-and-biases/sympathetic-magical-thinking-the-contagion-and-similarity-heuristics/
- https://my.clevelandclinic.org/health/diseases/9490-ocd-obsessive-compulsive-disorder
Our Review Standards
Our team regularly reviews health and wellness writings. Updates are made on the availability of new & authentic information.
Our Editorial Team
Clinical Adviser:
Author:



