
Bipolar depression is a mood state within bipolar disorder, unlike MDD, is marked by prolonged low mood, loss of interest, and reduced energy. The key element is its tendency to a constant change of elevated or irritable mood (mania or hypomania).
These shifts affect sleep, activity, thinking, and judgment, and they can disrupt daily life. The condition is medical and treatable. Moreover, bipolar disorder can also co-occur with schizophrenia and other psychiatric conditions.
Types of Bipolar Disorder
- Bipolar I: At least one full manic episode; depressive episodes are common but not required for diagnosis.
- Bipolar II: At least one hypomanic episode and one major depressive episode; no history of full mania.
- Cyclothymic Disorder: Two or more years of fluctuating hypomanic and mild depressive symptoms that don’t meet full episode criteria.
- Other Specified/Unspecified: Clinically significant mood elevation and depression that don’t fit the above patterns.
Find Stability From Home
Get expert care for bipolar depression through CPG’s secure telepsychiatry, same-day appointments across New Jersey, with in-clinic follow-ups when needed. Personalized plans for medication, therapy, and routine support.
Recognizing Bipolar Depression Symptoms
Whether it is social anxiety disorder (SAD), seasonal affective disorder (SAD), persistent depressive disorder (PDD), major depressive disorder (MDD), or Bipolar depression, the key to the right recovery path is the expert evaluation by the certified psychiatrists and psychologists. It is also very important to know about the comorbid conditions to avoid any misdiagnosis.
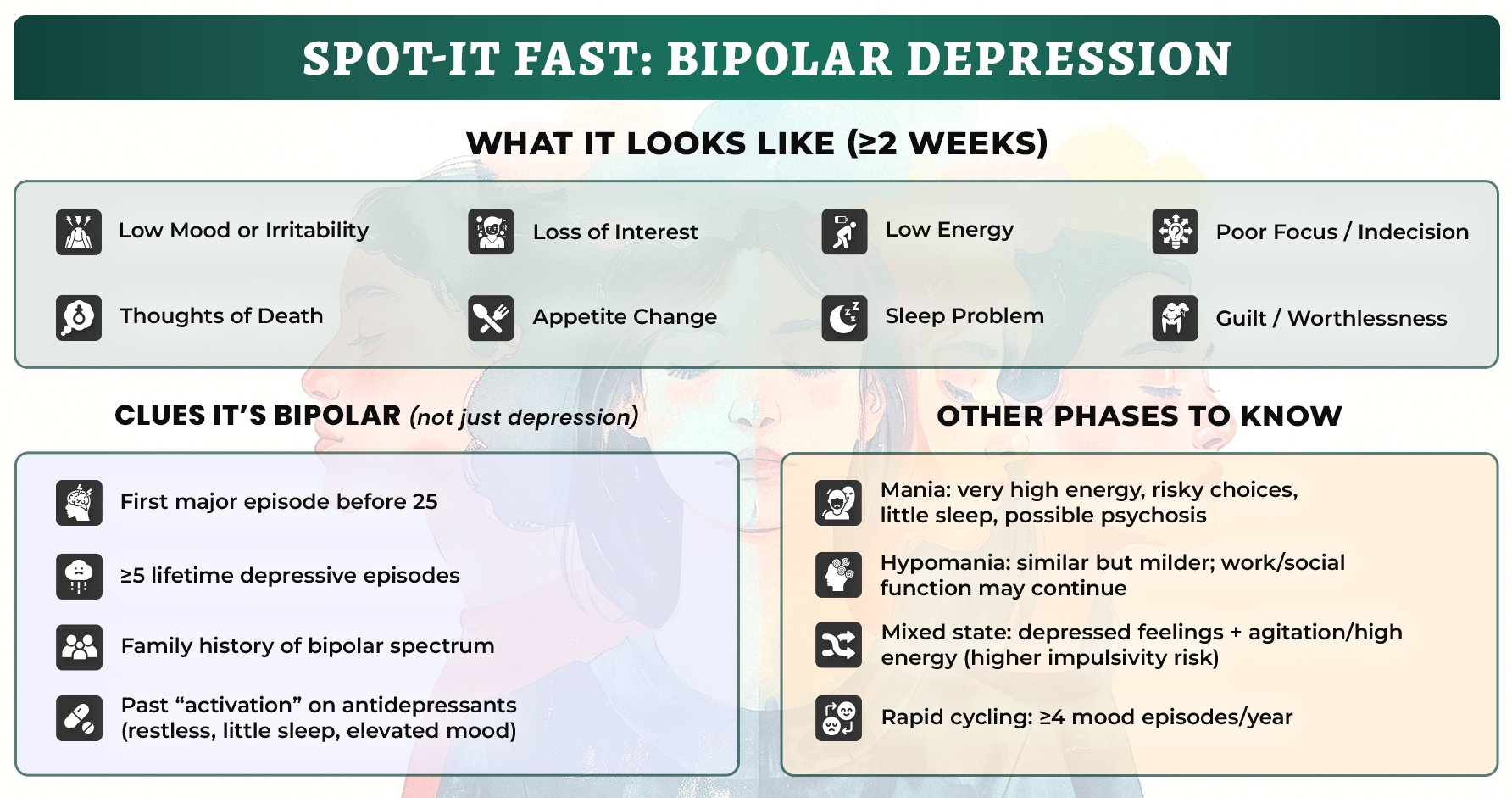
Core symptoms (≥2 weeks)
- Persistent sadness, emptiness, or irritability
- Noticeable loss of interest or pleasure
- Fatigue or low energy
- Sleep change (insomnia or hypersomnia)
- Appetite/weight change (loss or gain)
- Slowed thinking, slowed movements, or agitation
- Trouble concentrating, forgetfulness, and indecision
- Feelings of guilt, worthlessness, or hopelessness
- Thoughts of death or suicide
Pattern Suggesting Bipolar Depression Rather than Unipolar
- First depressive episode before age 25
- Five or more lifetime depressive episodes
- Family history of bipolar spectrum illness
- Antidepressant-induced restlessness, reduced sleep, or mood elevation in the past
Subtle Early “tells” Before a Drop
- New-onset fatigue with either insomnia or oversleeping
- Short bursts of push or talkativeness that fizzle quickly
- Tight focus flipping into indecision within days
Cognitive and functional impact
Forgetfulness, slowed speech, decision paralysis affecting school or work, even when the mood looks “flat.”
Expert Insight
- Within three years of an initial unipolar depression diagnosis, about 20–30% may shift to a bipolar pattern; subthreshold hypomanic symptoms occur in up to ~40% of recurrent depression
- Youth may show faster mood shifts, irritability over visible sadness, somatic complaints (headache, stomachache)
Mania, Hypomania, Mixed Features
Mania (often needs urgent care)
- Elevated or irritable mood with increased energy
- Rapid speech, racing thoughts, distractibility
- Less need for sleep
- Risky or impulsive behavior; grand plans
- Possible psychosis (delusions, hallucinations)
Hypomania (milder, no psychosis)
- Similar bipolar depression symptoms with less impairment; work/social function may remain intact
- Often followed by a depressive episode
Mixed Features (urgent risk)
- Depressive feelings with agitation, restlessness, and high energy
- Higher impulsivity and self-harm risk
Rapid Cycling
- Four or more distinct mood episodes in 12 months; more common in women and often driven by depressive phases
Want to Get Same-Day Telepsychiatry for Bipolar Depression?
Licensed psychiatrists/Psychiatrists, discreet video visits, and fast medication management, without travel or waiting rooms. Physical clinics are available if a face-to-face visit is the better fit.
Causes & Risk Factors of Bipolar Depression
Biology & Brain Function
- Strong heritability; multiple genetic loci involved
- Neurotransmitter and circuitry changes (dopamine, serotonin; altered connectivity; subcortical and cortical measures)
- Signals involving neurotrophic, mitochondrial, inflammatory, oxidative-stress, and HPA-axis pathways
Life Events & Environment
- Sleep–wake disruption (shift work, jet lag), bereavement, relationship breakdown, job loss, childbirth
- Early-life maltreatment (especially emotional abuse/neglect) is linked to later onset
Substances & Comorbidity
- Alcohol and recreational drugs worsen the course; dual-diagnosis care may be required
- Common medical comorbidities: thyroid disease, migraine, metabolic, and cardiovascular conditions
Course & Impact
- Global prevalence near 0.5% (≈37 million people)
- Average life expectancy reduction ~13 years, driven by medical illness and suicide risk
- Stigma and misdiagnosis remain common; timely care improves outcomes
Diagnosis & Evaluation
- Bipolar disorder is a clinical diagnosis based on history, symptom patterns, and collateral information when available.
Screening Aids (to prompt full evaluation):
- Mood Disorder Questionnaire (MDQ)
- Hypomania Checklist-32 (HCL-32)
Rule-out Workup when Indicated
- Urine drug screen; CBC/smear; CMP; thyroid function; B-vitamins/folate
- Review recent medication changes (e.g., steroids, stimulants), endocrine or neurologic illness
Specifiers to Capture Course and Risk
- Rapid cycling; seasonal pattern; anxious distress; melancholic features; peripartum onset; psychotic features (absent in hypomania)
Expert Insight
Many are diagnosed 6–10 years after first clinical contact; family/partner input can clarify past hypomanic or manic symptoms.
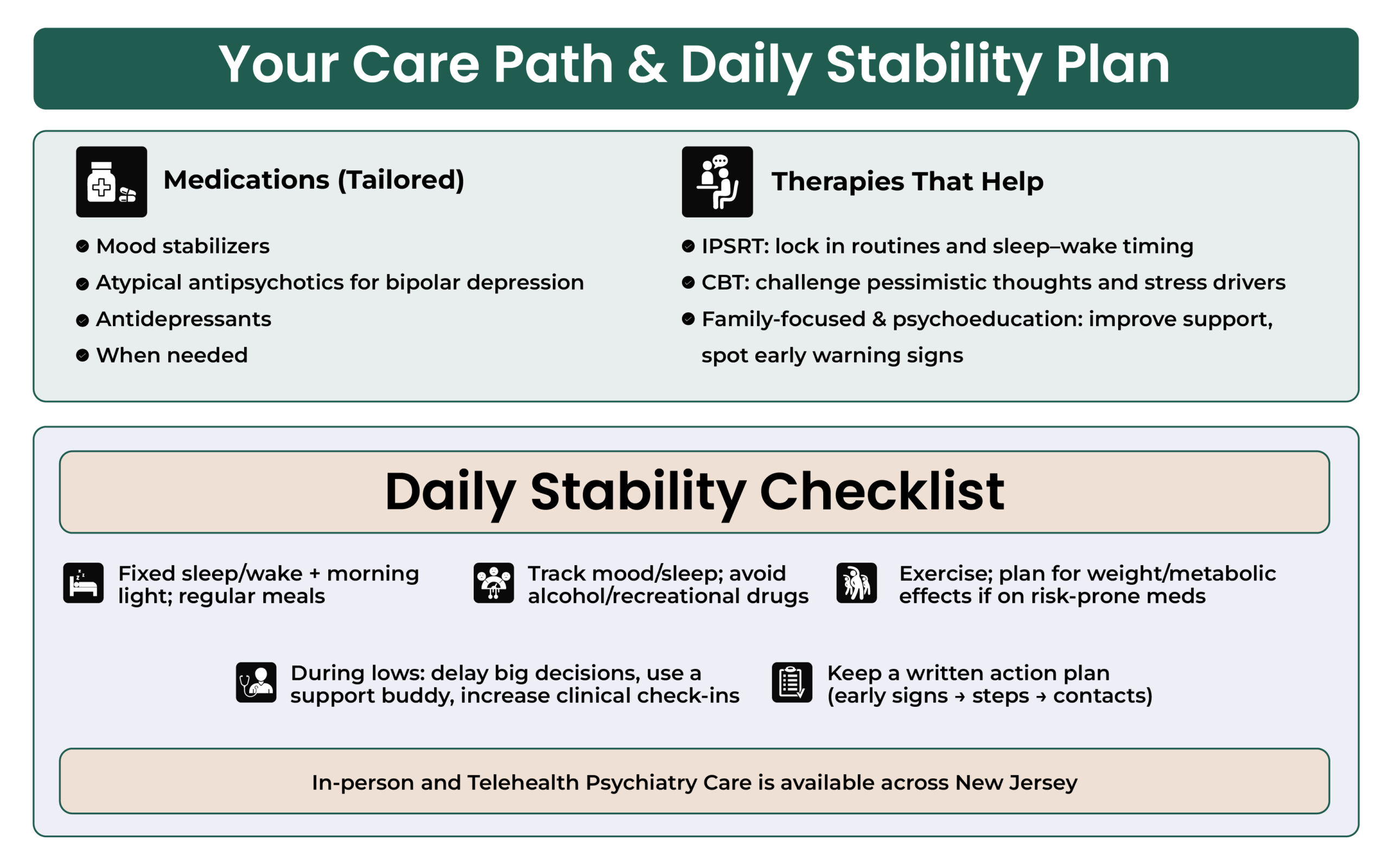
Bipolar Depression Treatment Options
A) Bipolar Depression Medications
Mood stabilizers
- Lithium: Broad relapse prevention and suicide-risk reduction; monitor serum levels, kidney and thyroid; educate on sodium loss and toxicity signs (blurred/double vision, irregular pulse, very slow/fast heart rate, breathing difficulty, confusion/dizziness, severe tremor/convulsions, passing large amounts of urine, uncontrolled eye movements, unusual bruising/bleeding).
- Valproate/divalproex: Effective for mania and mixed states; avoid in pregnancy and in people who can become pregnant.
- Lamotrigine: Strong for depression treatment and prevention; slow titration to reduce serious rash risk.
- Carbamazepine: Option in select cases with interaction and lab monitoring considerations.
Atypical Antipsychotics with Evidence in Bipolar Depression
- Quetiapine, lurasidone, cariprazine, olanzapine–fluoxetine combination
- Others are used as adjuncts when needed
Antidepressants
- Not used as monotherapy in bipolar disorder
- Consider only with a mood stabilizer or atypical antipsychotic, and close monitoring for switching
Augmentation and Special Situations
- ECT for severe, psychotic, or medication-resistant depression and for acute dangerous mania (including perinatal cases)
- TMS for refractory bipolar depression
- Thyroid augmentation in selected bipolar depression rapid cycling presentations
- Ketamine infusions for short-term antidepressant and antisuicidal effects when conventional options fail
CPG offers Care with Medication & Therapy Aligned
Evidence-based mood stabilizers and targeted psychotherapy (CBT, IPSRT), paired with sleep and mood tracking for steady progress. Ongoing check-ins to adjust quickly and keep you on course.
Bipolar Depression Therapy & Skills for Management
- Interpersonal and Social Rhythm Therapy (IPSRT): Stabilizes routines and sleep–wake timing
- Bipolar Disorder Cognitive Behavioral Therapy (CBT): Targets pessimistic thinking, stress responses, and relapse drivers
- Family-Focused Therapy & Psychoeducation: Improves communication, supports adherence, and sharpens early-warning detection
- Relapse prevention toolkit: Mood/sleep charting, personalized early-warning checklist, written action plan shared with supports
- Light therapy for bipolar depression is an effective treatment because of the fast improvements in symptoms.
Lifestyle & Safety Measures for Bipolar Depression
- Fixed sleep–wake schedule; anchor light exposure and mealtimes
- Avoid alcohol and recreational drugs; coordinate dual-diagnosis care when needed
- Regular exercise for mood and metabolic health; plan for weight-gain mitigation with medications that carry metabolic risk
- During depressive phases: postpone major life decisions; enlist a support person for medications and appointments; increase check-ins
CPG Care Model: Telehealth First, Clinics as Needed
Capital Psychiatric Group (CPG) provides on-site & telepsychiatry across New Jersey for assessment, medication management, and therapy. Care includes:
- All insurances are accepted
- Same-day & weekend appointments
- Walk-in appointments
- Therapy-first approach
- Structured follow-ups
- Therapy & counseling
- HIPAA-compliant Telepsychiatry
- In-person clinics are available
Get Back to Your Day: Manage Bipolar Depression Now
Video visit on your schedule, clear next steps, and fast medication adjustments when needed. Stay at work or home while we handle the clinical details.
FAQs
What’s the difference between bipolar depression and major depression?
Some symptoms may overlap, but bipolar depression occurs within a pattern that also includes hypomania or mania. History of mood elevation, antidepressant-induced activation, early onset, and family history support a bipolar pattern.
Do You Accept Same-Day Appointments?
Yes, Capital Psychiatry Group offers on-site & telehealth services across New Jersey State, and same-day appointments are accepted.
Can antidepressants be used?
They are not used alone; when considered, they are paired with a mood stabilizer or atypical antipsychotic and monitored for switching.
How common is rapid cycling?
Defined as four or more distinct episodes in 12 months, it’s more frequent in women and usually driven by depressive phases.
Do people recover?
Yes. Recurrence is common, but with the right plan, medication, therapy, and routine, most people achieve long-term stability.
How we reviewed this article:
CPG experts follow strict sourcing standards, using peer-reviewed research, academic institutions, and trusted medical journals. Only reliable, evidence-based sources are cited to maintain accuracy and integrity.
- https://my.clevelandclinic.org/health/diseases/9294-bipolar-disorder
- https://www.who.int/news-room/fact-sheets/detail/bipolar-disorder
- https://pubmed.ncbi.nlm.nih.gov/15780695/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2671727/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4615936/
- https://pubmed.ncbi.nlm.nih.gov/15780695/
- https://www.healthline.com/health/bipolar-disorder/cognitive-behavioral-therapy
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7061484/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9484534/
Our Review Standards
Our team regularly reviews health and wellness writings. Updates are made on the availability of new & authentic information.
Our Editorial Team
Clinical Adviser:
Author:



