
Capital Psychiatry Group offers psychiatric care throughout New Jersey, providing in-clinic appointments and telehealth services. This guide explains what a specific phobia is, the full picture of specific phobia symptoms, how clinicians diagnose it using DSM-5 specific phobia criteria and ICD-10 specific phobia codes, and which specific phobia treatments reliably reduce fear and avoidance.
What is a specific phobia?
A specific phobia is a persistent, out-of-proportion fear of a particular object or situation that triggers immediate anxiety or panic and leads to avoidance or distressed endurance. The fear lasts months or longer, interferes with work, school, or relationships, and many people have more than one phobia.
Unlike ordinary nerves before a test or speech, anxiety disorder-specific phobia typically does not fade on its own and often continues if left untreated.
Types and Everyday Examples
Clinicians group specific phobias examples into five standard categories:
- Animals: dogs, snakes, spiders, insects, rodents.
- Natural environment: heights, storms, deep water, darkness.
- Blood-injection-injury: seeing blood, getting shots, dental or medical procedures.
- Situations: flying, driving, bridges or tunnels, enclosed spaces, elevators, visiting the dentist.
- Other: choking, vomiting, loud sounds, clowns, costumed characters.
Common labels include acrophobia (heights) and claustrophobia (confined spaces). People often carry multiple fears across categories.
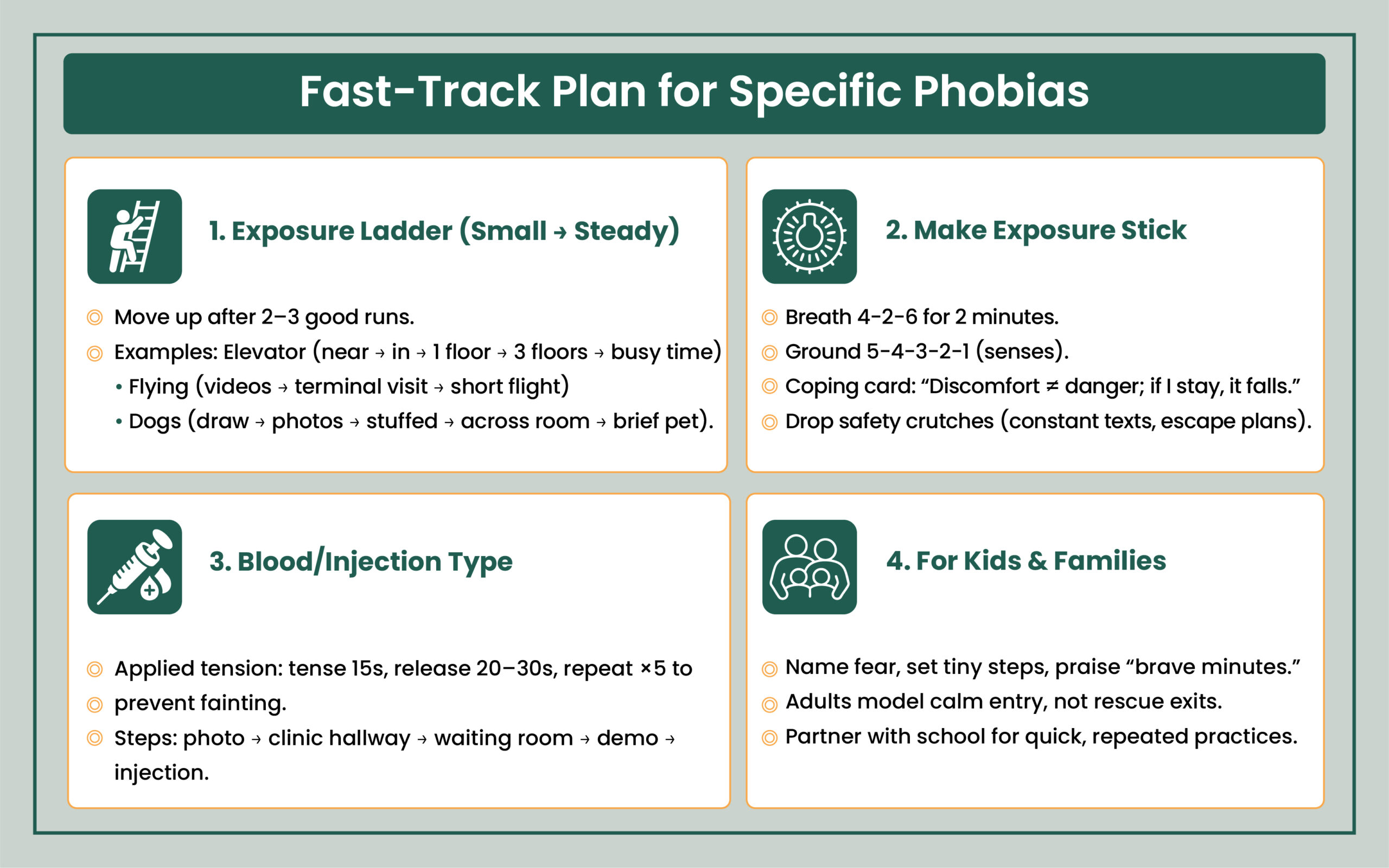
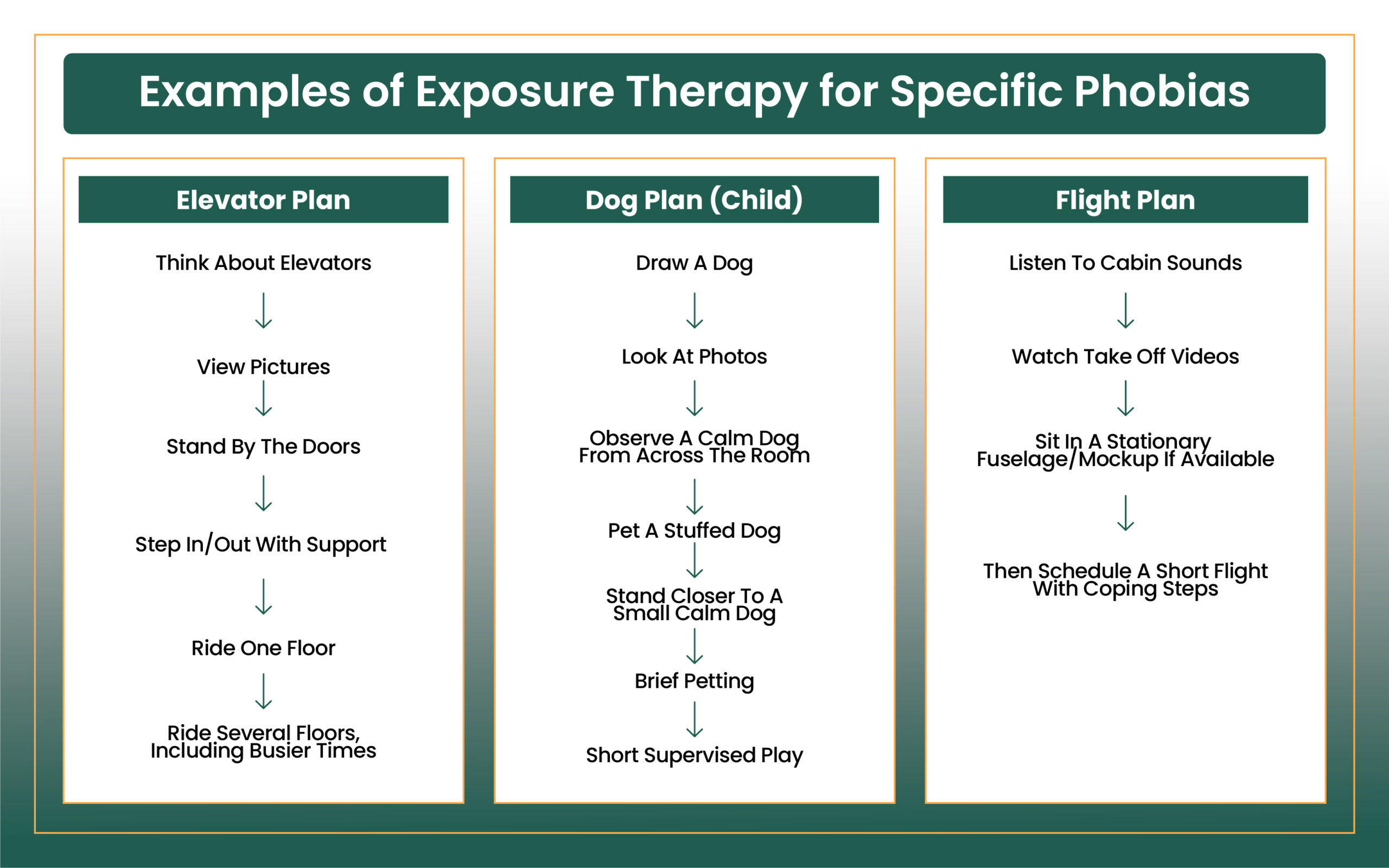
Make Elevators, Needles, Flights Doable
Build a short exposure ladder with a clinician and practice steps you can repeat this week, not someday. We’ll coach breathing, applied tension, and “stay-till-it-drops” timing, which you can use in real life.
How Common is it?
Specific phobia statistic: about 8%–12% of people in the U.S. meet criteria at some point; worldwide estimates are 2%–6% overall. Rates are 3%–9% in children and about 16% in teens, then decline in older adults. Women are affected about twice as often as men. Adult-onset phobias tend to persist, and only a small fraction remit without care.
Symptoms of Specific Phobias You May Notice
Mental and Emotional Symptoms
- Intense or overpowering fear, a need to escape, or the feeling of being in immediate danger when exposed, or even when thinking about the trigger (anticipatory anxiety).
- Knowing the fear is excessive, yet unable to control it.
- In severe moments, feelings of detachment from oneself or surroundings (depersonalization/derealization).
Physical (Including Panic-like Reactions) Symptoms of Phobias
- Rapid heartbeat, chest tightness, shortness of breath.
- Sweating or chills, trembling or shaking.
- Nausea, stomach upset, or diarrhea; feeling like choking.
- Dizziness, lightheadedness, tunnel vision, pallor.
- Numbness or tingling in hands/feet.
- With the blood-injection-injury type, fainting can occur because of a vasovagal drop in blood pressure.
Behavioral Symptoms of Specific Phobias
- Avoidance (skipping elevators, flights, medical or dental care).
- Life rearrangement to minimize any chance of encountering the trigger.
- Enduring unavoidable situations with extreme distress.
Child-Specific Symptoms
- Crying, clinging, freezing, tantrums, or refusing to approach the feared situation. Children may not recognize the fear as unrealistic.
One-Off Fear Coming Up?
Big presentation, MRI, or flight ahead—use targeted skills plus event-day supports (beta-blocker when appropriate) to get through without avoiding. Book a quick consult to map a precise, time-limited plan.
DSM-5 Criteria and ICD-10 coding
DSM-5 specific phobia criteria require:
- Marked fear or anxiety about a specific object/situation that almost always provokes immediate anxiety.
- Avoided or endured with intense distress; fear is out of proportion to actual risk.
- Duration ≥ 6 months, with clear distress or functional impairment.
Expert Insight
Use Applied Tension, Not Avoidance
- If you get light-headed around needles or blood, fainting risk is tied to a drop in blood pressure; counter it with applied tension.
- Sit or lie down, then tense thighs, glutes, and core hard for 10–15 seconds, relax 20–30 seconds; repeat 5 cycles before and during the procedure (resume if you feel warm, gray vision, or nausea).
- Build graded exposure in between appointments: images → videos → holding an empty syringe → alcohol swab smell → tourniquet on → saline practice with a clinician.
- Hydrate, eat a light salty snack beforehand, and tell staff so they can position you safely and pace the steps.
Why it Happens: Causes and Risk Factors
Always remember that no single cause explains all cases, but several pathways (genetics, severity of symptoms, stimulants, family history, substance, parenting, etc) contribute:
- Direct traumatic learning: a frightening event or a panic attack in the situation can spark a lasting fear.
- Vicarious and informational learning: witnessing another’s trauma or repeatedly hearing alarming stories can build a strong danger signal.
- Family patterns: a blend of genetics and learned responses; children pick up fear from caregivers who react anxiously or become overprotective.
- Temperament: high anxiety sensitivity, negative affect, and difficulty tolerating bodily sensations.
- Brain function and structure: phobic cues activate specific circuits more strongly in people with phobias; structural/functional differences are reported between individuals with and without certain phobias.
- Age and sex: onset commonly occurs in childhood (by ~10 years), can also begin in adolescence or adulthood; women are affected more often.
- Avoidance maintains the cycle: staying away brings short-term relief but reinforces the belief that the situation is dangerous, so anxiety grows over time.
Resolve Blood/Injection Fainting Fears with CPG
Learn applied tension, graded exposure, and clinic walk-throughs so you can get labs, vaccines, and dental care without passing out. A few focused sessions can change the pattern.
Possible Complications if Untreated
- Social isolation and missed opportunities (declining jobs that require travel, avoiding celebrations in tall buildings, postponing needed procedures).
- School and work problems, reduced independence, and family strain from constant reassurance-seeking or protective accommodations.
- Higher rates of depression, other anxiety disorders, and substance misuse.
- In severe cases, the risk of suicidality rises.
- Avoiding medical settings can delay important care.
How Clinicians Make the Diagnosis
A clinician reviews triggers, avoidance patterns, duration, and impact, plus medical and mental health history. They may use brief questionnaires. There’s no lab test; diagnosis is clinical using DSM-5. For children, input from parents/teachers clarifies functional impairment at school and home.
Evaluation also separates specific phobia from conditions like Generalized Anxiety Disorder, panic disorder, or trauma-related disorders.
Treatments at CPG that Work
First-line: Exposure Therapy
The most effective treatment is exposure therapy which changes the learned response to the feared situation. Therapy proceeds in graded steps from least to most difficult, with repeated practice until anxiety recedes. Exposure can be:
- In vivo (real-life practice).
- Imaginal when real exposure is unsafe or impractical (supplemented by pictures, video, or virtual tools).
Cognitive Behavioral Therapy (CBT) Skills that Support Exposure
- Identify catastrophic predictions (“the elevator will fall,” “I’ll faint and never recover”) and test them against the actual situation.
- Practice tolerating bodily sensations (racing heart, dizziness) without escape behaviors.
- Learn breathing control and progressive muscle relaxation to settle physical arousal during exposure.
- Build behavioral experiments that show you can ride, fly, or get an injection and have the anxiety pass without avoidance.
Medications: When and how they’re used
- Beta-blockers (e.g., propranolol) can blunt pounding heart, shaky voice, tremor for time-limited events like public speaking or a one-off flight.
- Benzodiazepines may reduce acute anticipatory anxiety, but they’re used sparingly and short-term due to dependence risk; not recommended for those with substance-use histories.
- SSRIs are not routine for isolated specific phobia; they may be considered when a phobia co-occurs with depression or broader anxiety disorders (e.g., Generalized Anxiety Disorder) or when exposure work isn’t feasible.
- For the blood-injection-injury type with fainting, therapists teach applied tension (brief muscle tensing to maintain blood pressure) alongside exposure.
Lifestyle and Home Strategies that Help
- Mindfulness and relaxation (deep breathing, yoga) to manage arousal while you practice staying in the situation.
- Regular physical activity, consistent sleep, and limiting caffeine can intensify bodily sensations.
- Do not rely on reassurance loops or extensive online searching; both keep avoidance in place.
- Gradual approach: remain near the feared situation with support instead of detouring completely; frequency matters more than duration, short, regular exposures build progress.
Help Your Child Face Fears with CPG
We’ll set tiny, brave steps for school, shots, dogs, or dark and show you how to praise approach, not avoidance. Parent coaching + school notes make daily practice simple.
Helping a Child with Specific Phobia
- Talk openly about fears; don’t minimize or shame.
- Avoid reorganizing life around the fear; instead, use small, supported steps toward the trigger and praise brave actions.
- Model calm coping: show your own plan for facing a feared situation and how you recover from anxiety.
- If school attendance, sleep, or social life are affected, seek a child therapist skilled in exposure and response prevention; medication is rarely needed in children for an isolated specific phobia.
Coping and Support for Specific Phobias
- Practice what you learn in therapy between sessions; build a written plan for flare-ups.
- Reach out to a support group or trusted person who understands you’re working on staying in the situation rather than escaping it.
- Celebrate gains, even small ones (one floor in the elevator, a minute in the waiting room, holding the needle cap).
Expert Insight
Do “micro-exposures” daily (1–5 minutes) to keep
- momentum: one elevator ride, a short bridge crossing, a brief video of flying, small wins add up.
- Replace reassurance loops with a plan: set a worry timer (e.g., 10 minutes), do the exposure, then log the result; if you still want to Google or ask for reassurance, wait 30 minutes and re-rate your urge.
- If your phobia triggers panic-like sensations, add interoceptive practice (jog in place, spin gently, hold your breath briefly) so body sensations stop feeling like danger.
- For one-off events (an MRI or flight), rehearse with videos or on-site walk-throughs; if a beta-blocker is prescribed, test it on a calm day first and avoid sedatives that can blunt exposure learning.
Prevention and Early Action
Phobias arise unpredictably. You can’t guarantee prevention, but early intervention after a frightening event reduces the chance that avoidance hardens into a phobia. Parents who address their own fears with treatment are less likely to model avoidance that children may copy.
When to Seek Care and When to Seek Urgent Help
If you rearrange your days to avoid situations or you endure them with severe distress, treatment can help; earlier care leads to stronger results. If fear, depression, or substance use escalates, or if there are thoughts of self-harm, seek immediate support by calling or texting 988 in the U.S.
Online care with Capital Psychiatry Group
Capital Psychiatry Group offers online/in-clinic mental health services, serving communities across New Jersey with same-day appointments when available. Care includes assessment of specific phobia, structured CBT with exposure, coaching for applied tension in blood-injection-injury type, and thoughtful use of medications when indicated.
During evaluation, clinicians also screen for related conditions, Generalized Anxiety Disorder, Social Anxiety Disorder, and clarify Panic Disorder vs. Anxiety Attacks, so treatment matches the full picture.
Virtual Fear Lab: Practice From Home & Visit when You Want
Safe and guided exposures by video (elevators via parking garage cam, flight sims, needle walk-throughs) so you can rehearse skills where you feel secure. We’ll track anxiety drop curves and tweak steps in real time.
How we reviewed this article:
CPG experts follow strict sourcing standards, using peer-reviewed research, academic institutions, and trusted medical journals. Only reliable, evidence-based sources are cited to maintain accuracy and integrity.
- https://my.clevelandclinic.org/health/diseases/24757-phobias
- https://www.health.harvard.edu/diseases-and-conditions/common-triggers-of-vasovagal-syncope-and-how-to-reduce-your-risk-of-fainting
- https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t11/
- https://www.ncbi.nlm.nih.gov/books/NBK499923/
- https://www.mayoclinic.org/diseases-conditions/specific-phobias/symptoms-causes/syc-20355156
- https://www.sciencedirect.com/science/article/abs/pii/S0272735808000639
- https://www.mayoclinic.org/diseases-conditions/specific-phobias/diagnosis-treatment/drc-20355162
- https://988lifeline.org/
Frequently Asked Questions
What is a specific phobia?
A lasting, excessive fear of a particular object or situation that almost always produces immediate anxiety, leads to avoidance or distressed endurance, persists ≥6 months, and causes impairment.
Symptoms of a specific phobia?
Overwhelming fear, anticipatory anxiety, rapid heartbeat, chest tightness, nausea or diarrhea, shaking, tunnel vision, dizziness or fainting (especially with needles/blood), and avoidance. Children may cling, freeze, cry, or have tantrums.
DSM-5 criteria for specific phobia / DSM 5 specific phobia criteria?
Marked, immediate fear tied to a specific trigger; out-of-proportion risk; duration ≥6 months; impairment; not better explained by another condition.
Specific phobia ICD-10 code / ICD-10 specific phobia?
F40.2x, with subtype noted (animal, natural environment, blood-injection-injury, situational, other).
Panic disorder vs specific phobia?
In a specific phobia, panic is cue-bound (tied to a trigger). In panic disorder, attacks are unexpected, with ongoing worry about future attacks and behavior change. Both can co-occur and are treated differently.
Prevalence of specific phobia?
Overall, 8%–12% in the U.S.; 2%–6% worldwide; 3%–9% of children and ~16% of teens meet criteria; rates decrease with age. Women are affected more often.
Treatment for specific phobia / specific phobias treatment?
Exposure therapy (systematic, repeated practice) is the cornerstone. CBT adds thought and behavior skills. Beta-blockers or short-term benzodiazepines may help for rare, unavoidable events; daily SSRIs are considered when there is broader anxiety or depression. Relaxation and mindfulness support exposure work.
Does “panic disorder vs. anxiety attacks” matter for care?
Yes. Anxiety attacks in specific phobia are tied to a particular situation; panic disorder requires a different plan emphasizing interoceptive exposure and relapse prevention. Your clinician will sort this out at intake.
Is there a cure?
Most people improve markedly with exposure-based therapy. Many can ride, fly, get shots, or enter enclosed spaces with manageable anxiety and no longer rearrange life to avoid the trigger.
How is this different from Social Anxiety Disorder or Generalized Anxiety Disorder?
Social Anxiety Disorder centers on fear of scrutiny or embarrassment in social or performance settings. Generalized Anxiety Disorder involves broad, persistent worry across life areas. Specific phobia is targeted at one object or situation.
Looking for specific phobia therapy “near me” in NJ?
Capital Psychiatry Group provides in-clinic & telepsychiatry services statewide with structured CBT for specific phobias and coaching for real-world exposures you can practice at home or in your community.
Our Review Standards
Our team regularly reviews health and wellness writings. Updates are made on the availability of new & authentic information.
Our Editorial Team
Clinical Adviser:
Author:



