
Not all, but many females notice mood and physical changes before their period. Premenstrual dysphoric disorder (PMDD) (previously known as LLDD) is different. It’s a severe, long-lasting form of premenstrual syndrome that brings specific mood shifts, irritability, or anger. Additionally, there are clear physical symptoms like bloating, breast tenderness, headaches, and overwhelming fatigue.
These problems appear in the week or two after ovulation, peak just before bleeding, and ease within a few days of menstruation. During that window, day-to-day life is severely impacted: work performance slips, conflicts rise at home, and normal routines feel unmanageable.
What is Premenstrual Dysphoric Disorder (PMDD)?
Premenstrual dysphoric disorder is a severe, chronic form of premenstrual syndrome that appears in the late luteal phase and eases within a few days after bleeding starts. It disrupts day-to-day functioning at home, school, work, and in relationships. Lifestyle changes help many people; some will also need medication or structured therapy.
The Week Before Feels Unbearable?
If the days before your period derail work, sleep, and relationships, you don’t have to push through it alone. CPG offers same-day online/in-clinic PMDD care across New Jersey.
Is PMDD Treatable?
The good news: PMDD is treatable. Options include lifestyle adjustments, targeted premenstrual dysphoric disorder treatments such as SSRIs (continuous or luteal-phase dosing), and hormonal contraception regimens; supplements and structured stress management can support recovery.
Capital Psychiatry Group delivers evidence-based therapy, counseling, and medication management services online and in-person, so you can start a plan that fits real life. If symptoms raise safety concerns, urgent help comes first; ongoing care then focuses on steady relief.
Expert Insight
- SSRIs: Luteal-only for mood/irritability; daily if somatic symptoms dominate, reassess after 1–2 cycles.
- Hormonal options: Drospirenone/EE (continuous or short placebo) if eligible.
- Pair meds with aerobic exercise, sleep regularity, caffeine/alcohol cutbacks, and brief CBT skills.
- If partial response: consider venlafaxine, targeted sleep support, and coordinated psychological services through CPG.
How PMDD Differs from PMS
Both Premenstrual Syndrome (PMS) and PMDD bring premenstrual physical complaints (bloating, breast tenderness, headaches). Whereas, PMDD adds increased mood and behavioral symptoms, irritability, intense anxiety, depressed mood, sudden tearfulness, and feeling out of control. PMDD is listed in DSM-5 as a depressive disorder.
Who Is at Risk of Premenstrual Dysphoric Disorder
- Family history of PMS/PMDD or mood disorders.
- Personal history of depression, postpartum depression, anxiety, or trauma.
- Smoking & lower access to education about premenstrual management.
- Stress, overweight/obesity noted as contributors in some reports.
Mood Swings Keep Blindsiding You?
Trackable patterns deserve a real plan. Get a targeted PMDD evaluation, treatment options (CBT, SSRIs, hormonal), and follow-ups, all by telehealth and in-house clinics with Capital Psychiatry Group.
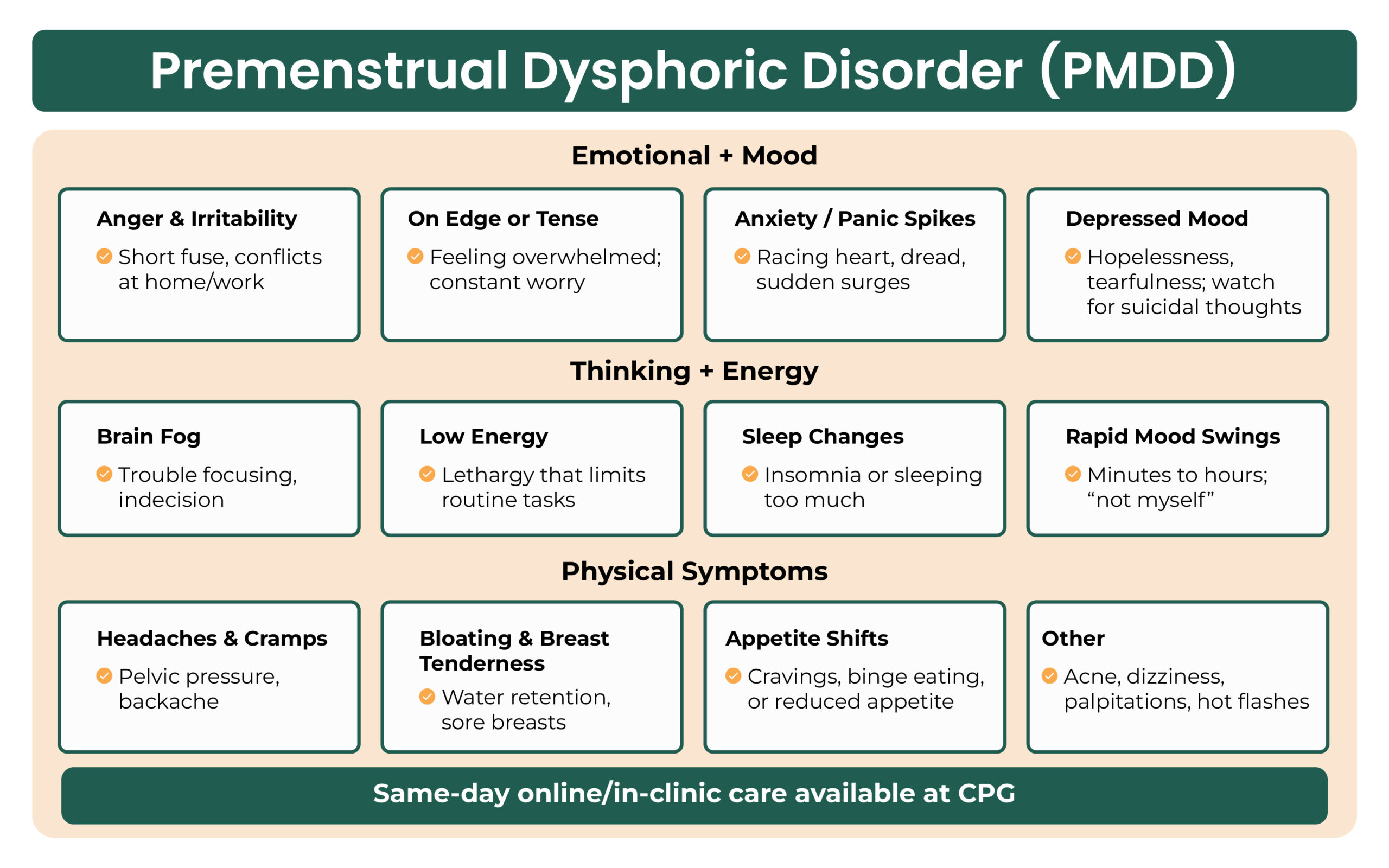
Common Symptoms of PMDD (emotional, physical, cognitive)
Timing: Begin a week or two before menses; resolve within several days of the onset of bleeding. For some, symptoms recur every cycle until menopause.
Mood/behavior Symptoms
- Marked irritability or anger; conflict with others
- Sudden mood swings; frequent or sudden tearfulness
- Persistent anxiety, panic spikes, tension
- Depressed mood, hopelessness, and self-critical thoughts
- Feeling overwhelmed or out of control; low interest in activities
- Sleep change (insomnia or sleeping more); fatigue, low energy
- Reduced libido, food cravings, binge eating, and appetite change
Cognitive Symptoms of PMDD
- Difficulty concentrating, increased forgetfulness, and mental fog
Physical Symptoms
- Breast swelling/tenderness, bloating, and pelvic heaviness
- Headaches, joint or muscle aches, and backaches
- Weight gain or fluid retention (hands/feet/ankles), diminished urine output
- Nausea, constipation, or other GI upset
- Dizziness, faintness, palpitations, tingling, or heightened sensitivity in limbs
- Skin changes (acne, itching, flares of other conditions)
- Hot flashes; muscle spasms
Expert Insight
- Confirm pattern: daily ratings × 2 cycles (late-luteal spike, relief after menses).
- SSRIs: luteal-phase for mood; daily if fatigue/sleep/pain dominate; reassess in 1–2 cycles.
- Hormonal option: drospirenone/ethinyl estradiol (continuous/short placebo).
- Rule out thyroid/anemia; differentiate PMS, major depression, bipolar depression, seasonal affective disorder.
- Safety: screen suicidality pre-menses; set a brief crisis plan and tighten follow-ups.
Why It Happens: Current Understanding According to Research
The exact cause isn’t fully known. Current evidence points to a heightened sensitivity to normal monthly hormone changes, with downstream effects on serotonin, the brain chemical tied to mood, sleep, and appetite.
PMDD is more likely when there’s a personal or family history of PMS or mood disorders (including depression or postpartum depression), exposure to major stress or trauma, or cigarette smoking; some people also face barriers to education about management and care.
The Role of Co-occurring Conditions in PMDD
Up to one in ten females who menstruate may meet the criteria. Because PMDD shares features with other conditions, such as major depressive disorder (MDD), seasonal affective disorder, persistent depressive disorder (PDD), bipolar depression, postpartum depression, ADHD, and generalized anxiety, careful diagnosis matters for the recovery.
Tracking symptoms across two cycles, ruling out thyroid and other medical issues, and confirming that at least five symptoms (with one mood symptom) recur in the late luteal phase helps clarify the picture.
Diagnosis & Screening (including DSM-5 points)
Diagnosis is clinical, based on history and prospective daily ratings across at least two cycles. A physical and pelvic exam helps exclude other causes; thyroid disease and primary anxiety/depression should be considered.
DSM-based Approach (condensed):
- In most cycles over the past year, ≥5 symptoms present in the final week before menses, improving within a few days after onset, minimal in the week post-menses.
- At least one mood-related symptom (e.g., marked lability, irritability/anger, depressed mood, anxiety/tension).
- Clear distress or impairment in social, work, or other areas.
- Not better explained by another disorder or solely an exacerbation of an existing condition.
Need Relief Before Day 21?
Set up a cycle-specific plan: symptom tracking, step-by-step coping skills, and medication if needed. Meet a CPG clinician online/in-person this week and steady the month ahead.
Evidence-Based Treatments for PMDD
Treatment plans are customized; our expert psychologists and psychiatrists combine lifestyle measures with medication or structured therapy. Capital Psychiatry Group delivers these options through online psychological services with same-day starts when needed.
First-line Medications
Note: This is not medical advice and is not equivalent to the doctor’s observations.
- SSRIs (sertraline, fluoxetine, escitalopram, citalopram, and paroxetine HCl in selected cases) improve mood, irritability, anxiety, energy, sleep, and cravings.
- Dosing options: continuous daily or luteal-phase only (from ovulation to menses). PMDD often responds faster than major depression, making intermittent dosing feasible for some.
- Common early effects (e.g., nausea) tend to fade; sexual side effects may persist and should be discussed.
- SNRIs (e.g., venlafaxine) are reasonable alternatives when SSRIs are not effective or tolerated.
Hormonal Options
- Combined oral contraceptives (e.g., drospirenone/ethinyl estradiol; continuous or shortened hormone-free interval) can decrease both physical and mood symptoms by stabilizing hormonal fluctuations.
Self-Care & Lifestyle Supports
- Regular aerobic activity supports mood and energy.
- Diet shifts: smaller, more frequent meals; ease back on caffeine, alcohol, excess sugar, and salt.
- Sleep routine and light refreshing habits; relaxation, mindfulness, or yoga.
- Plan for the high-symptom window by reducing avoidable stressors and setting realistic workloads.
CPG’s Online and In-Clinic Care Model
Capital Psychiatry Group (CPG) provides telepsychiatry & on-site care for evaluation, medication management, and therapy. We coordinate with mental wellness clinics and primary care when required
What to Expect in PMDD Care
- All insurances are accepted
- Weekend & walk-in appointments
- Same-day appointments
- HIPAA-compliant telepsychiatry
- Accessible clinics across New Jersey
- Thorough history and cycle-linked symptom review
- Clear plan (luteal vs continuous SSRI, contraceptive options, symptom-targeted aids).
- Expert psychiatrists & psychologists
- Therapies and first-liners are prioritized
Is It PMDD or “Just PMS”?
Get a clear answer with a focused screening, two-cycle symptom tracking, and a personalized plan (therapy, meds, lifestyle) via telehealth/onsite clinics across New Jersey. Same-day appointments available, steady your next cycle.
How we reviewed this article:
CPG experts follow strict sourcing standards, using peer-reviewed research, academic institutions, and trusted medical journals. Only reliable, evidence-based sources are cited to maintain accuracy and integrity.
- https://womenshealth.gov/menstrual-cycle/premenstrual-syndrome/premenstrual-dysphoric-disorder-pmdd#
- https://www.webmd.com/women/pms/pms-vs-pmdd
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/premenstrual-dysphoric-disorder-pmdd
- https://my.clevelandclinic.org/health/diseases/9132-premenstrual-dysphoric-disorder-pmdd
- https://www.health.qld.gov.au/newsroom/features/breaking-the-cycle-a-guide-to-understanding-and-managing-premenstrual-dysphoric-disorder-pmdd
- https://www.ncbi.nlm.nih.gov/books/NBK532307/
Our Review Standards
Our team regularly reviews health and wellness writings. Updates are made on the availability of new & authentic information.
Our Editorial Team
Clinical Adviser:
Author:



